Information for professionals
Cheyne Child Development Service referrals and pathways
On this page
- How does it work?
- Referral criteria
- Easy access to the service
- Booking interpreters
- Can a parent or carer refer directly?
- Days and hours of operation
- Multi-agency intake meeting
- What this means for referrers
- What this means for families
- Child Development Services referral form
- What to expect from the service
- Information for GPs on ASD and ADHD referrals in Hammersmith and Fulham
- Moving out of area
- Moving into area
- Follow-up after an autism assessment
- School-aged ASD pathway
- Referrals not routinely accepted on the school-aged ASD pathway
- Referrals for 17 to 18-year-olds
- Challenging behaviour
- Dental referrals
- Dyslexia
- Dyscalculia
- Developmental language disorder
The Cheyne Child Development Service (CCDS) is a multi-agency service made up of local teams with expertise in child development (medical, nursing, therapies and clinical psychology). We support children and young people aged 0 to 19 years.
The service aims to make sure referrals are managed promptly and that children and young people are seen by the right professionals. Referrers should complete the referral form and attach any other relevant reports or documents.
The Child Development Service provides a strong and innovative service that supports children and young people and their families, including those in vulnerable groups such as children with disabilities, children with social paediatric needs (including adoption and looked after children) and children and young people with specific developmental health needs.
How does it work?
Parents and carers can ask a health professional or an education setting that knows their child to complete a referral form and send it to the Child Development Service.
Usually a GP, hospital clinician, school nurse, health visitor or SENCo will refer a child, with the parent or carer’s permission. Information is treated as confidential. It is normal practice for staff to share information with relevant professional colleagues involved in the child or young person’s care.
Referral criteria
To meet the criteria for Cheyne Child Development Service, one of the following must apply:
- Severe delay in one area of development, or
- Significant delay in more than one area of development
Cheyne Child Development Service supports children and young people aged 0 to 19 years who meet the criteria above and have a GP in one of the following postcode areas:
- Hammersmith and Fulham: SW6, W6, W12, W14, NW10 (partial)
- Kensington and Chelsea: SW6, W6, W12, W14, NW10 (partial)
- Westminster: SW1 only
Easy access to the service
- Local outreach in two hubs: Parkview Centre for Health and Wellbeing (Hammersmith and Fulham) and Chelsea and Westminster
- Local therapy service provision
- School clinics for vulnerable children at Jack Tizard
Booking interpreters
We can arrange an interpreter or translator to attend an appointment if needed, as long as we have notice in advance. Please let us know on the referral form if an interpreter is required, including the preferred language.
Can a parent or carer refer directly?
We do not currently accept parent or carer referrals for a child or young person’s first referral to Child Development Services.
Days and hours of operation
The service operates flexibly within normal working hours for the majority of services.
Multi-agency intake meeting
All referrals are discussed at a weekly multi-agency intake meeting. This meeting is attended by senior practitioners from Speech and Language Therapy, Physiotherapy, Occupational Therapy, Clinical Psychology, Neurodevelopmental Paediatrics and Community Nursing.
Each referral is reviewed and a decision is made based on the information provided. Decisions include:
- whether the referral is appropriate and can be accepted
- whether further information is needed
- which services are required
- which service will make the initial contact with the family
All referrals must relate to children and young people with a GP in our postcode areas and must only be made with the agreement of the parent or carer. Consent sections on the referral form must be completed.
What this means for referrers
- You only need to complete one referral form, even if the child needs access to several services
- Your referral will be considered by a senior multi-disciplinary and multi-agency forum
- If appropriate, involvement from additional services can be arranged without requiring further referrals
What this means for families
- It will be clear which service will make the initial contact
- Relevant services can accept the referral at the same time
- Families do not need to wait to see one service before joining another service’s waiting list (if appropriate)
If you are a professional working with children and are concerned about a child’s development, you can make a referral to the Child Development Service.
Child Development Services referral form
This referral form supports referrals for children of all ages, including pre-school and school-aged children. The form must be completed by professionals referring into the service.
Please complete the form digitally and submit it to the relevant service. Handwritten forms will not be accepted.
Information about Cheyne Child Development Service can be found under Specialist services.
What to expect from the service
- An assessment which may include investigation, diagnosis, treatment and early intervention, based on the child and family’s needs
- A flexible and responsive service committed to working in partnership with parents and carers, children and young people
- High quality information and support at the earliest opportunity to plan together with families
Information for GPs on ASD and ADHD referrals in Hammersmith and Fulham
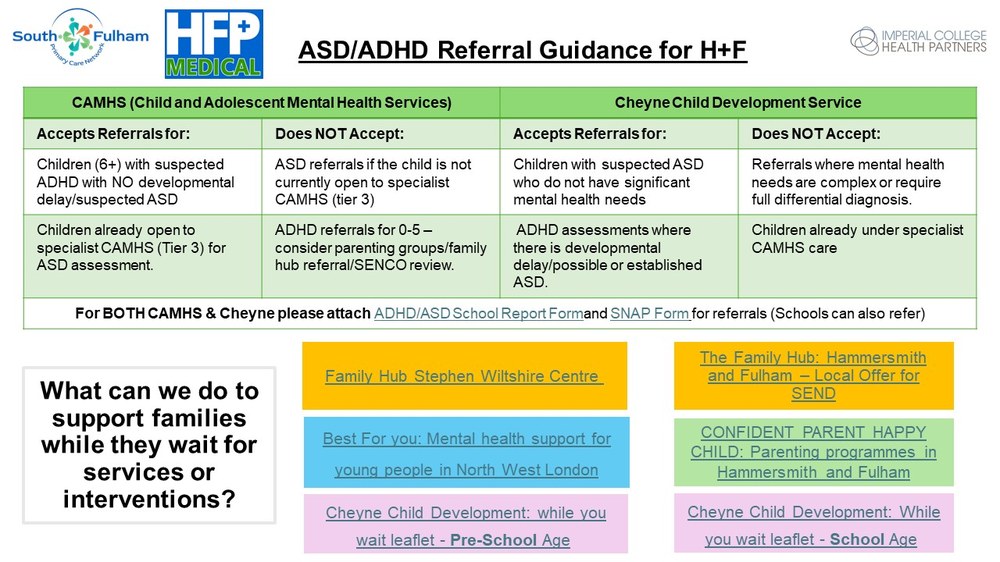
Please see our pages on autism and ADHD for more information.
Moving out of area
If a child moves out of area while on our waiting list, they can usually remain on the waiting list for an assessment as long as:
- The family wishes to remain on our waiting list and understands they will need to attend appointments in our area
- They understand they will be discharged to local child development services after the assessment for post-diagnosis follow-up and therefore will not be able to access our post-diagnosis offer
- We receive information from local services (for example, nursery or school functioning questionnaires or reports from local therapists). If this is not provided, we may need to transfer care to local child development services
Moving into area
If a family has been on a waiting list for an autism assessment in another area and is then accepted onto our waiting list, we are not able to take account of waiting times in other areas unless there are specific safeguarding concerns.
Follow-up after an autism assessment
All children who have an autism assessment are offered a post-diagnosis follow-up appointment:
- with the Clinical Nurse Specialist (for the pre-school ASD pathway), or
- with the Clinical Psychology team (for the school-aged ASD pathway)
We do not offer routine medical follow-up appointments for children with an autism diagnosis. Paediatric appointments are offered only if there is a medical need.
Please see our autism webpage for more information. (Add link)
School-aged ASD pathway
The CDS school-aged autism pathway accepts referrals for children and young people who attend primary or secondary school (aged 4 years 6 months to 18 years) and who present with:
- observable difficulties with social interaction
- delayed or atypical language development
- delayed or atypical pretend play and imagination
- difficulty adjusting to ordinary social demands and routines, including reduced flexibility around change or transitions and rigidity around routines
- concerns about behaviour such as repetitive behaviour, significant sensory-seeking behaviour, anxiety and phobias
- concerns about emotional regulation, or reduced ability to feel reassured by parents or carers
The child’s presentation and the level of concern will vary depending on their developmental level, their age, whether they have additional neurodevelopmental syndromes (such as fragile X) and whether there are social or emotional vulnerabilities present.
Children may enter and leave the pathway at any age. Access to services from the multidisciplinary team is led by the child’s assessed needs.
Key stages of the pathway include:
- educational transitions (for example, nursery to primary school, primary to secondary school)
- adolescence, due to an increased likelihood of additional mental health concerns such as anxiety and depression
Referrals accepted
- Children already known to the Child Development Service where concerns about social communication have emerged
- New referrals where information suggests social communication difficulties beyond the child’s developmental level
Referrals not routinely accepted on the school-aged ASD pathway
1. Significant mental health difficulties, risk or safeguarding concerns
- We will not accept referrals where there are significant mental health diagnoses such as an eating disorder, obsessive-compulsive disorder, serious risk of self-harm or involvement with forensic CAMHS
- We do not accept referrals where there is previous or current CAMHS involvement suggesting primary mental health difficulties within the family system related to the referral question
- Referrals that focus on pre-existing diagnoses given by CAMHS (for example ADHD or ODD)
2. Significant emotional trauma or attachment difficulties
- Referral information suggests a differential diagnosis of attachment disorder
- More complex social issues have been raised (for example neglect)
- Concerns about significant emotional trauma history where attachment disorder has not been excluded
- Where appropriate and with parent or carer consent, referrals may be redirected to CAMHS for assessment and intervention around trauma or attachment. If CAMHS later feel ASD assessment is indicated, they can complete the assessment themselves or refer to relevant tertiary services
3. Pathological demand avoidance (PDA) as a specific assessment request
- We do not diagnose PDA. We may describe a demand-avoidant profile as part of an autism assessment
4. Tics or Tourette syndrome assessment or management
5. Second opinion
- These referrals should be directed to tertiary services (for example Great Ormond Street Hospital)
Note: Referrals should be made by a professional working with the family (for example a GP or school).
Referrals for 17 to 18-year-olds
- We do not accept referrals for young people who will turn 18 within 3 months of the referral. In this situation, we advise the referrer to make a referral to the adult autism assessment team when the young person turns 18.
- We accept referrals for 17-year-olds but do not prioritise these. Our acceptance letter can explain that, given current waiting times, the young person is likely to turn 18 before reaching the top of the waiting list. At that point, we will contact them to gain consent and request updated information to redirect the referral to the adult autism team. Where possible, we will indicate how long the young person has been on our waiting list and ask the adult service to take this into account.
If there are mental health concerns, the child or young person should continue to access support through CAMHS while waiting. If anyone believes a child or young person is in immediate danger because of mental health concerns, please seek urgent advice from A&E or call 999.
Challenging behaviour
Please see our ‘Support while you are waiting for an autism assessment’ webpage for borough-specific information. (Add link)
Please also see our mental health support page. (Add link)
Kooth
Kooth is an online wellbeing community where young people aged 11 to 25 can chat with counsellors, keep an online journal, read articles written by other young people and connect through a moderated group. Kooth also has a neurodiversity section with useful resources.
EMBRACE group
The Cheyne Clinical Psychology team, along with Occupational Therapy, Speech and Language Therapy, Music Therapy and Specialist Nurses, run the EMBRACE group for parents and carers of children aged 0 to 7 years. The group focuses on understanding your child and making sense of their behaviour.
For more information, contact: chelwest.ccds.psychology@nhs.net
Charities supporting challenging behaviour
Dental referrals
For information about dental support for children with complex needs, including a list of resources, please see:
If a child has difficulty accessing a local dentist, they can be referred to Community Dental Services. Referrals can be made by health professionals such as the GP, dentist, paediatrician or Speech and Language Therapist. Referrals are also received from the school nursing team.
Central London Community Healthcare NHS Trust
Referral Management Centre
Soho Centre for Health and Care
1 Frith Street
London
W1D 3QS
Email: clcht.dental@nhs.net
Telephone: 020 7534 6524 or 020 7534 6529
Dyslexia
Dyslexia may be suspected when a child does not develop literacy skills despite appropriate intervention. If a parent is worried about their child’s progress with literacy (reading, spelling and writing), the first step is to speak to the child’s school and raise concerns with the class teacher or SENCo.
All state schools can provide support and intervention to help children develop literacy skills. In some situations, where school-based intervention is not effective, schools can access specialist literacy support for further advice.
A formal report diagnosing dyslexia is not needed to access support in local schools.
For more information, visit the British Dyslexia Association:
For more support with working with schools, see:
Dyscalculia
Dyscalculia may be suspected when a child does not develop numeracy skills despite appropriate intervention. If you are worried about your child’s progress with numeracy, the first step is to speak to your child’s school and raise concerns with the class teacher or SENCo.
All state schools can provide support and intervention to help children develop numeracy skills. In some situations, where school-based intervention is not effective, schools can access specialist support for further advice.
A formal report diagnosing dyscalculia is not needed to access support in local schools.
For more information, visit the British Dyslexia Association:
For more support with working with schools, see:
Developmental language disorder
Developmental language disorder (DLD) is a common condition, affecting around 7% of the population, but it is often under-recognised.
DLD is a communication disorder where children and young people have difficulties understanding and using spoken language. It can affect speaking, listening, reading and writing. It can interfere with learning, understanding and using language at school, at home and in everyday life.
DLD persists into adulthood and can have a significant impact on social interactions, educational progress and emotional wellbeing.
Language difficulties in DLD are not explained by other conditions, such as hearing loss or autism.
DLD has also been called specific language impairment, language delay or developmental dysphasia.
A child or young person who speaks more than one language will have difficulties in all of their languages.
How DLD is diagnosed
A Speech and Language Therapist can assess a child for DLD. If there are other developmental concerns, a paediatrician may be involved as part of a multi-disciplinary assessment.
DLD can co-occur with other conditions such as ADHD and dyslexia.
How to support children with DLD
Focus on the child’s strengths and support their needs. Many people with DLD are socially motivated and, with the right support, can build friendships and take part in their community.
Speech and Language Therapy can support children and families with practical strategies after diagnosis. Teachers can support children by adapting teaching approaches, for example using visual or pictorial instructions.
Videos
Darcie, a young girl with DLD, shares her story:
Lily, a young woman with DLD, explains what it is like to live with the condition:
Further reading and support
Support for young people and families is available from:

