Gastric banding
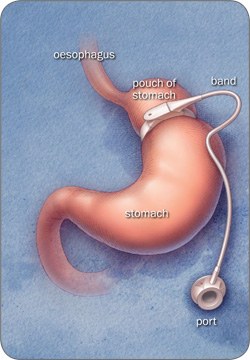
The band creates a narrowing between the top and bottom part of the stomach. The band is filled with fluid via a port (small chamber) placed under the skin.
This stops the food from passing quickly into the stomach, keeping food sitting in the pouch. The food stimulates the nerves at the top of the stomach to give you a feeling of fullness.
You should fill up quickly, and stay full for longer, even after only a small amount of food (the amount eaten by a toddler).
The stomach and intestines are not cut, stapled or removed when placing the band. Therefore digestion and absorption are not affected.
If you need further operations in the future, the band can be removed and the original shape of the stomach will return to normal.
The band is not filled with fluid at the time of surgery. Your first band fill will usually be about 6 weeks after surgery. These procedures are performed in X-ray or in the outpatients department and take up to 30 minutes.
You may need your band tightened more than once, to create the correct amount of restriction from the band. Your dietitian or surgeon will discuss this with you, based on your food intake, eating skills and weight loss.
Expected weight loss
You will tend to lose weight steadily over 2 years following surgery. On average, people lose about 50–60% of their excess body weight.
There is, however, a large variation in results and weight loss is not guaranteed. Adherence to dietary advice is necessary to achieve these results.
The dietitian will discuss with you what changes you would need to make to your eating patterns to have the best weight loss results.
Advantages
- The amount of food you can eat is restricted
- You may feel fuller quicker and stay fuller for longer
- The band can be adjusted to increase or decrease the restriction via the access port under the skin on your stomach
- You can lose on average 50–60% of your excess weight
- The surgery itself has fewer risks than the Roux-en-Y gastric bypass and the sleeve gastrectomy, because it is a shorter procedure and the stomach and intestines are not cut, stapled or removed
- The stomach and intestines remain intact so food is digested and absorbed as normal
- The surgery can be reversed (although you will probably regain the weight
Disadvantages
- Weight loss is slower than following the Roux-en-Y gastric bypass or the sleeve gastrectomy
- Weight loss may not start until many months after surgery, until the band is filled to the optimum level for your stomach
- The surgery will not always create the feeling of fullness
- The access port may twist so be inaccessible for band fills—you may require another operation to correct the problem
- The port or band may leak and deflate, which may require another operation to correct the problem
- The band may move or slip (2–5% of cases)—you may need to have all the fluid removed from your band for a period of time, or need another operation to remove or replace it
- The band may erode into the stomach wall and need another operation to remove or replace it (1% of cases)
- The band or port may become infected and need to be removed
- You may suffer from worsening gastro-oesophageal reflux (heart burn), ulceration, gastritis, bloating, difficulty swallowing, dehydration and constipation
- Nausea and vomiting may occur, particularly in the first few days after surgery—vomiting is also common if you eat too quickly or eat too much
- 10% of people fail to lose the expected amount of weight with the band
- For successful weight loss, you will have to follow dietary changes and have self control
Should you require any other type of emergency or elective surgery in the future, the gastric band should not cause any problem.
However, the surgeon performing the operation must be informed about your gastric banding prior to surgery.

