Treating the Flat Foot
General
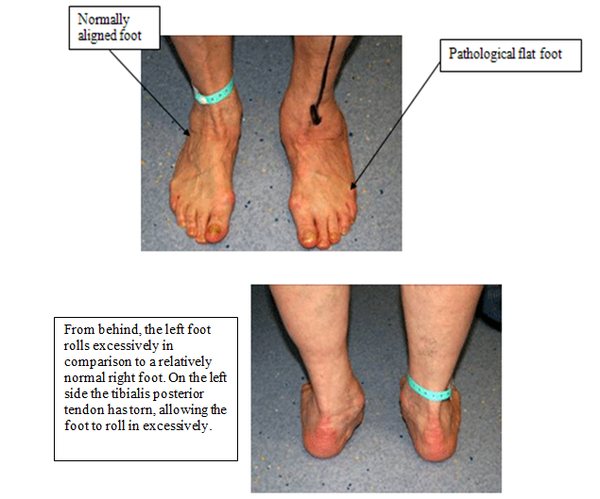
A flat or low arched foot is not considered abnormal, the height of the arch does not have any bearing on how well a foot can function. However, a foot that rolls in excessively with most of the weight passing over the inside border is a cause for concern, as shown in the left foot pictured below.
Treatment is required in severe cases or where the degree of mal-alignment is such that the patient experiences pain or fatigue, or is likely to do so.
These patients are considered to have a pathological flat foot. In the majority of cases the symptoms respond to stretching exercises, orthoses (shoe inserts) and supportive footwear. If the patient does not respond to conservative treatment, then surgery might be considered.
Causes of a pathological flat foot
- Deformity present at birth
- Tendon injuries, typically Tibialis posterior
- Diseases that affect muscle and nerve function
- Joint hypermobility
- Abnormal joining of two bones (coalition) resulting in a rigid flat foot
- Arthritis
Types of abnormal flat feet
The pathological flat foot can be divided into flexible and rigid, and whether it is an adult or child. The diagnosis is made by a clinical examination of the foot and the patient’s gait. The causes as outlined above are varied and investigations are often required in the form of X-rays and scans to confirm the severity and underlying causes.
The diagnosis will be given to you during your outpatient appointments along with the treatment options and the likely outcomes.
Treatment options
Conservative care
Stretching exercises for the calf and hamstring muscles
- Having tight calf muscles has been shown to increase the likelihood of the foot collapsing (arch height reducing and the heel bone rolling in). An improvement in flexibility can normally be achieved by standing on an adjustable slant board for 2-3 minutes twice a day, indefinitely.
Physiotherapy to strengthen muscles and improve coordination
- An individual programme of exercises would be needed, although the major muscle groups are the core, thigh and buttocks
Orthoses (Insoles), ankle braces
- These devices help hold the foot in a neutral position when walking. They do not cure the poor alignment, but if used they can provide support, although they are generally only effective in laced training shoes.
Managing pain
- Anti inflammatories and analgesics
- Local steroid injections
Supportive shoes
- If the shoe is to provide support it needs to reduce unwanted motion. Therefore, it needs to be fairly stiff and to be held firmly to the foot with laces that are securely fastened.
Ankle Brace

Calf Stretch board
Orthoses

Hoka walking shoe
Surgical Management
Surgery should only be considered if conservative care has failed, except when the deformity arises from an acute injury such as a fracture or tendon rupture.
The operation normally involves a combination of techniques to restore the alignment of the foot to the lower leg. This includes osteotomies (cutting bones to re-align them), fusing joints, tendon lengthening and transfers as well as implanted devices to help maintain correction.
The outcome and approach will depend on whether the foot position is fixed or rigid and whether you are a child or an adult. The best outcomes are in children with a flexible foot.
Children
Flexible pathologically flat foot
Here the foot is poorly aligned when standing, but when sitting with the weight off the foot the deformity corrects itself. In general, lateral column procedures (Evans) have been the mainstay of surgical intervention with good reliable outcomes in the literature.
This is often combined with lengthening of the calf muscle, when stretching has failed to provide adequate flexibility. In some instances, in order to support the arch additional soft tissue procedures are performed and this may be combined by fusing two bones (Hoke procedure).
Likely procedures or combinations:
- Evans
- Arthroereisis
- Navicular cuneiform fusion (Hoke)
- Lengthening of the calf tendon
Rigid pathologically flat foot
Here the foot remains in a poor position irrespective of whether it is weight bearing or not. This could be due to arthritis, the abnormal joining of two bones (coalition) or a birth defect.
The surgery might be simple when the coalition is between the navicular and the calcaneum with excision of the bony bar. In complex cases the surgery may involve fusing major joints, leading to improved position but a stiffer foot.
The procedures here will depend on the diagnosis and will be given to you following your consultation
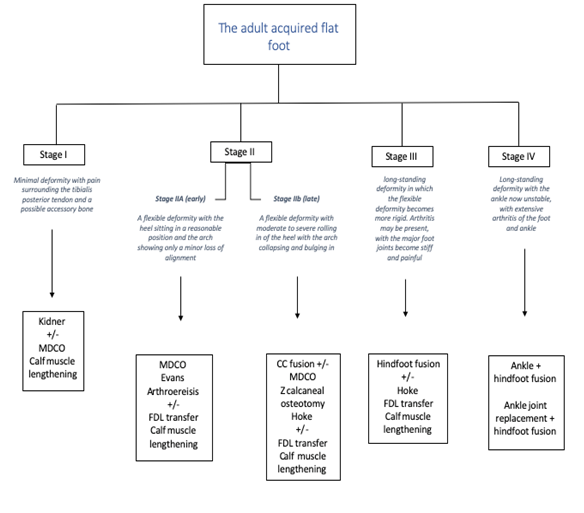
The adult acquired flat foot
The causes of the adult flat foot are varied and depending on how long the patient has suffered from this complaint, arthritis in the foot joints may have developed. This generally leads to a poorer outcome, with patient’s generally experiencing a reduction in pain along with a more stable foot, although it is likely to be stiffer post-operatively.
The flow chart below offers some of the possible surgical solutions as the foot goes from minor changes to severe with arthritis
Lengthening of the calf tendon
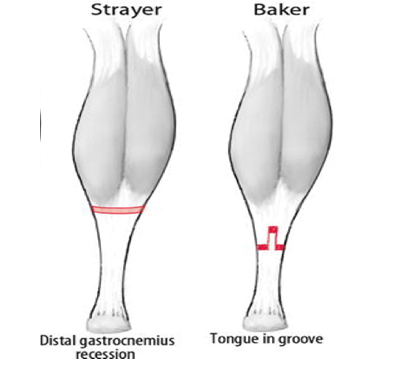
The two common approaches are the Strayer or Baker. Lengthening of the tendon allows normal foot function but the calf is often weaker and smaller than the other side. Rarely the sural nerve is irritated leaving numbness or hypersensitivity to the lower leg.
Kidner
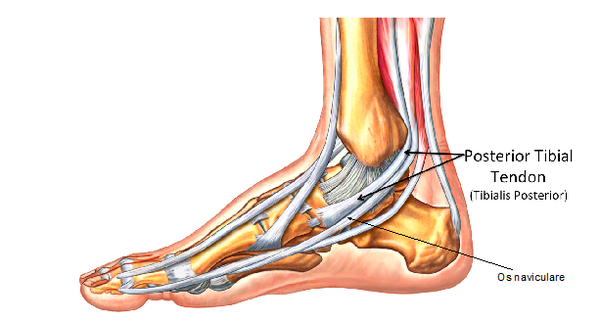
The surgery here shortens the tendon and removes the accessory bone. The incision runs from around the ankle to the midfoot. In very mild cases this procedure might be performed in isolation or combined with other soft tissue and bone procedures.
FDL Tendon transfer
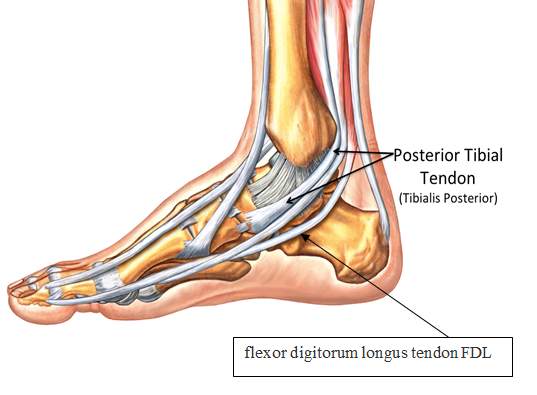
The torn tendon would consequently be replaced by a nearby tendon (flexor digitorum longus tendon FDL). This tendon can be used without greatly affecting lesser toe function as there is another tendon which performs almost the same job within the foot.
FDL would be used to replace the torn tibialis posterior tendon. The FDL muscle and tendon is approximately one third of the size of tibialis posterior. Consequently, performing this procedure in isolation would fail to provide long term stability and correction.
Spring ligament repair or augmentation
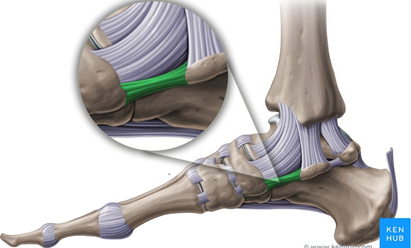
The spring ligament (in green) connects the navicular bone and the heel bone (calcaneus) and helps prevent the foot from collapsing in.
In feet that have been poorly aligned for years, this ligament can stretch or tear, causing pain and severe deformity. When appropriate the ligament can be repaired or augmented with an implanted fibre wire to support the arch. It is a procedure that is rarely performed in isolation, but as part of a combination of techniques to correct the foot position.
Calcaneal (heel bone) osteotomy (MDCO)
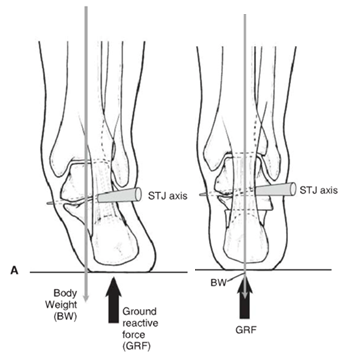
Moving the heel back into a neutral position helps reduce the forces pushing the foot into a pronated or poor position. When the heel is moved into a neutral position the calf muscle has greater leverage in controlling the position of the foot.
Arthroereisis
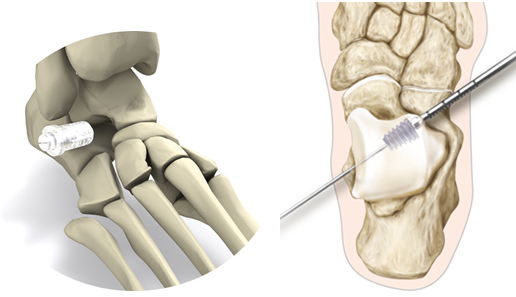
When the foot rolls in this gap reduces in size and expands when the foot rolls out. By placing the right size implant in the sinus tarsi, we can limit the amount of rolling in (pronation) of the foot.
This implant is not always tolerated by the patient and in some cases, it has to be removed. It is unlikely that an arthroereisis would be used in isolation. NICE guidelines in 2009 recommended caution with regard to the use of this device as the long-term data on its efficacy and potential complications was not known.
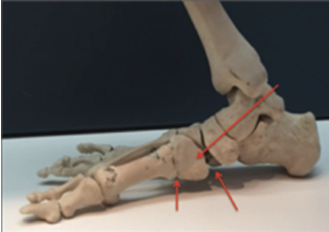
Evans Calcaneal osteotomies
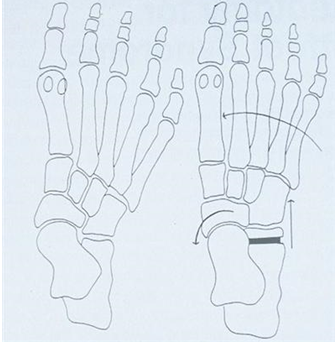
This procedure lengthens the outside of the foot in cases where the foot has become severely mal-aligned. The procedure is normally reserved for children or in adults with a degree of hypermobility and no signs of arthritis.
The use of this procedure has been well documented in the scientific literature, with good long-term outcomes in children who are generally more adaptable than adults. It has been shown to be a powerful tool in correcting the flat foot deformity, although in adults it can lead to arthritis forming in some of the joints on the outside border of the foot.
The heel bone is cut and a bone graft taken and reinserted to lengthen the lateral border of the foot, increasing the arch height and stabilising the foot. It does not fuse any joints and the major movements of the foot are preserved, although the direction of movement is changed to prevent excessive rolling in of the foot.
Calcaneocuboid distraction arthrodesis
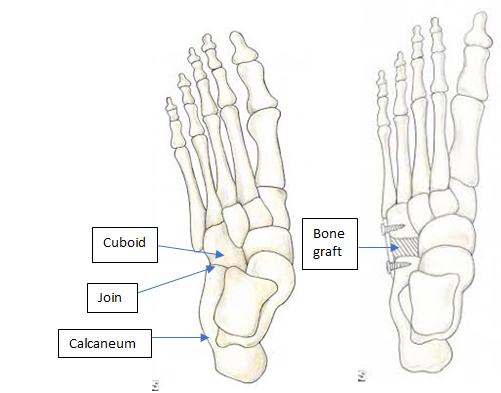
In adults, lengthening the lateral border of the foot remains very effective in correcting a flat foot. However, the traditional Evans procedure is not always well tolerated with arthritis sometimes developing in the adjacent calcaneocuboid joint. This approach lengthens the lateral border of the foot by fusing the calcaneocuboid joint using a bone graft, preventing arthritis from occurring in this joint.
The downside is a stiffer foot and some patients still complain of pain affecting the lateral border of the foot. The fusion site can also be painful if the bones do not unite with the risk being around 2-4%.
Rotational calcaneal osteotomy
This procedure combines some of the advantages of the Evans and the MDCO providing an increased ability to realign severe mal-alignment without fusing any joints.
There remains the risk in the adult patient of developing arthritis in other foot joints, depending on how well the individual adapts to the foot being repositioned. Other risks include nerve and tendon irritation due to the increased dissection and the proximity of these structures.
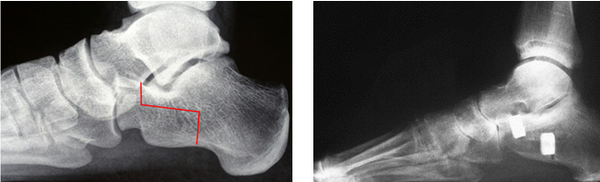
(Pre and post X-rays showing the line of the bone cuts and subsequently view post procedure with the calcaneum lengthened and rotated at the same time)
Hoke (Navicular cuneiform fusion)
The pathological flat foot tends to sag at the navicular cuneiform joints. Given time the loss of alignment is fixed, often with arthritis present. Taking a wedge to correct the arch and reduce the instability is a common adjunctive procedure providing good stability to the arch.
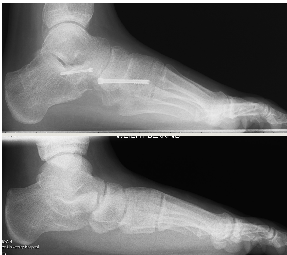
These X-rays show the foot from the side with initially a loss of arch height and a midfoot sag, in a young adult. Post procedure the lateral column has been lengthened using an Evans procedure with a navicular cuneiform fusion.
This has now been successfully realigned.
Fusions of the major foot joints

In cases where the foot is rigid a fusion of part or all of the major joints in the foot might be considered, to restore alignment and stability.
The ankle is not included allowing the foot to move up and down, but the rolling in and of the foot would be restricted. These operations are effective in correcting deformity, but the foot will be stiff as a result.
The ankle joint in later years can develop arthritis as it compensates for the reduced movement within the foot joints. This trade off must be viewed in the context of the pre-operative pain that the patient was experiencing and the damaging effect of the poor foot position on the other major joints.
Severe ankle and foot deformity

When left unchecked the poor foot position can sometimes lead to the ankle becoming unstable and potentially arthritic. When arthritis and severe deformity affects both the foot and ankle, this often fails to respond to footwear changes and bracing.
Given these findings, a major fusion of the foot and ankle is often required. The model shows a nail used to fuse the ankle and foot into a neutral position. Whilst this obliterates movement patients can compensate to a degree in the smaller joints of the foot assuming these are not too arthritic.
Post-surgery patients can walk in an orthopaedic shoe with a rocker type sole to provide the movement that would normally be available at the ankle joint.
Preoperative Assessment
Prior to having a general anaesthetic, you would be reviewed by the nurses to ensure that you were fit and well. You will be given all the relevant information on general anaesthesia and the opportunity to ask questions.
Day surgery
These operations are normally carried out on a day care basis. You would be admitted to the hospital on the day of your operation and shown to the ward. A member of the team will confirm your consent form and mark the surgical site.
General Anaesthesia
You will be put to sleep by the anaesthetic team for the duration of your operation waking up in recovery.
In addition, a local anaesthetic block in the back of your knee (Popliteal block) will be administered. This will numb your foot and lower leg providing pain relief for the 12 to 36 hours following the operation. It will also temporarily block your ability to move your foot and toes.
In adult patients the popliteal block is often performed prior to you being put to sleep. As the anatomy behind the knee varies a little from person to person, a nerve stimulator is used to accurately identify the nerves. This sends a small electric current down the needle so that when the nerve is approached it is stimulated. This means that the muscles controlled by that nerve begin to contract and relax causing the foot to ‘flick’.
If you are conscious it is a strange sensation, but it helps us to deliver the anaesthetic around the nerve with precision.
Reducing the risk of a blood clot (DVT)
Being in a cast and non-weightbearing places you at an increased risk of developing a DVT, if the clot travels to the lung (pulmonary embolism) this could be fatal.
You will be shown how to inject a drug (low molecular weight heparin) using a very small needle into the fat around your tummy. This thins the blood reducing the risk of you developing a DVT. The needle is very fine and for most patients it is not painful, it can leave a bruise, so we recommend that you move the injection sites around your tummy. These injections will need to be continued whilst you are in a cast non weightbearing.
The operation
The operation normally lasts for approximately 90-120 minutes with a cast put on the leg in theatre whilst you are asleep. The cast will start from just below your knee to your toes allowing us to maintain correction whilst the body is healing, reducing the likelihood of damage. Dissolving sutures will be used to close the skin.
Recovery
You must rest with the leg elevated for the first 48hrs (essential ambulation only). It is important that you keep the cast clean and dry.
X-rays will be taken to ensure good position and stable internal fixation and at 8 and 12-weeks signs of bone healing. A Limbo cast cover can be bought to enable bathing without getting the limb wet and increasing the risk of infection.
For some patients an additional partial weight bearing cast is applied for 4 weeks. The length of time you are in a cast for depends on the procedure and how well you are healing.
Returning back to activity and regular footwear is gradual and very much depends on the type of operation, your body’s healing response and the individual’s level of motivation.
Full recovery takes 7-12 months
Possible complications
Approximately 700 patients undergo foot surgery annually within the Department of Podiatric Surgery at West Middlesex University Hospital.
Most patients have an uneventful recovery. Outlined below are the common problems or those rare complications with serious outcomes. In cases where we don’t have accurate audit, we have used published results from the podiatric literature. These are accompanied by an asterisk *
- Prolonged swelling taking more than 6 months to resolve occurs 1 in every 500 operations*
- Haematoma – a painful accumulation of blood within the operation site. No recorded incidents.
- Thick and or sensitive scar – no audit data is available.
- Screws and plates were removed from 118 patients during a twelve-month period. This is often planned but can occur as a result of irritation.
- Adverse reaction to the post-operative pain killers. 1 in every 50 patients report that the codeine preparations can make them feel sick.*
- Infection of soft tissue. The incidence is 1 in every 83 operations*
- Infection of bone occurred in 3 out of 916 patients.
- Delayed healing of soft tissue or bone. No audit data is available.
- Circulatory impairment with tissue loss occurred in 3 out of 9000 patients over a 10 year period.
- Loss of sensation can occur although this is usually transient but can take up to a year to resolve.
- Deep vein thrombosis which can result in a clot in the lung is potentially a life-threatening condition. Within the published literature, the overall incidence of VTE is thought to be 0.9% in foot and ankle surgery.
- Chronic pain syndrome: this is where the nervous system dealing with pain over reacts in a prolonged manner often to a minor incident. This normally requires management by specialists in this condition and doesn’t always resolve. This is a rare complication with no audit data available.
- Reoccurrence of the deformity or failure of the operation
- Development of secondary problems including overloading of joints adjacent to the ones operated
The risk of having a complication can be minimised when the patient and all those concerned with the operation and aftercare work together. This starts with the pre-operative screening and continues through to the rehabilitation exercises.
Pre-operative screening of your health allows us to determine whether you are fit for surgery. It is important that you disclose your full medical history.
If there is a query regarding your health, then further investigations or the advice of other surgical and medical specialties will be sought. The surgeon and the theatre team will ensure that the operation is performed effectively and with the minimum of trauma.
You can improve the healing process and reduce the risks of complications by:
- Adhering to the post-operative instructions which include resting and elevating the operated leg. Keeping the wound clean and dry until advised otherwise is essential. Please ask the team if you are not sure what to do.
- Having a healthy diet is important. This provides the nutrition required for healing.
- Smoking is associated with a 20% increased risk of delayed or non-healing of bones.
- Alcohol can interact with the drugs that we will prescribe and in excess can impair wound healing.
- Post-operative exercises and in certain cases physiotherapy will be advised. This helps improve the flexibility, strength and stability of your foot.
Podiatric surgeons evaluate, diagnose, prevent and treat diseases, disorders and conditions affecting the foot and all associated structures. This is carried out in keeping with the individual’s education, training and experience, in accordance with the ethics of the profession and applicable law.
Podiatric surgeons are not medical doctors.
Podiatric Surgical Training
- 3 year: Degree in Podiatry (BSc)
- 2 year: Masters in the theory of podiatric surgery (MSc)
- 2 year: Surgical training programme (Podiatric Surgical Trainee)
Final fellowship examinations (Podiatric Surgeon) - 3 year: Specialist training (Podiatric Registrar)
- Accreditation with the Faculty of Podiatric Surgery
- Consultant Podiatric Surgeon

