Dietary Guidance after Gastric Band Surgery
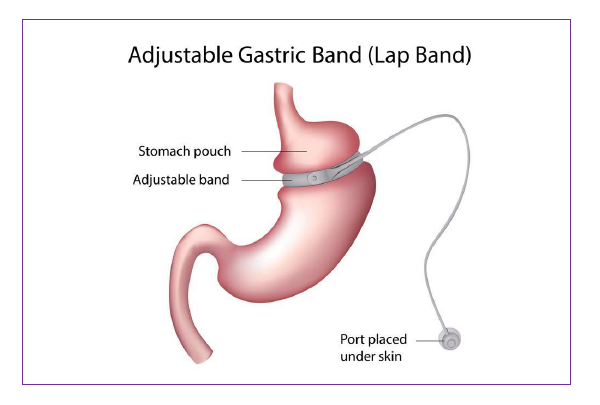
Introduction
This information will guide you through the post- operative stages step-by- step following insertion of a gastric band.
The texture progression phases from fluids to solids are important to reduce the risk of unpleasant side effects such as nausea, vomiting, pain and discomfort. The gradual texture progression also helps to avoid damage to your new stomach, allows your wounds to heal after surgery and allows food to pass easily from the stomach to your small intestine. It is important not to skip any of the stages.
You will need to follow a modified texture diet for 4 weeks, before returning to a regular texture diet. The diet is separated into 4 separate stages:
- Liquids
- Puree
- Soft
- Regular
The day after your surgery, your surgical team will tell you when it is safe for you to begin to sip fluids. A member of the dietetic team will see you before you go home to discuss the post-operative diet and answer any questions you may have.
Stage 1 – only smooth liquids for 1 week
All liquids should be completely smooth with no bits or lumps (e.g. can be sucked through a straw). Start with sips (little and often), and if you feel comfortable then gradually increase the amount. Avoid big gulps as this may cause discomfort, nausea, sickness and regurgitation.
Choose liquids that are high in protein to:
- help with wound healing and quicker recover
- prevent muscle loss
- keep you fuller for longer.
During this stage aim to have 1.5-2 litres of fluids each day to stay hydrated.
It is advisable to prioritise protein rich fluids over others such as tea, coffee etc.
Begin with sipping your drinks little and often and gradually increase the quantity until the sensation of feeling full occurs.
It is important to stop as soon as you feel full. If you drink too much, your stomach may overfill and cause pain, nausea and vomiting.
Which liquids are suitable?
Choose protein rich liquids at least 1 litre (2 pints) each day to help your body recover such as:
- Skimmed or semi-skimmed milk or lacto-free or soya milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes
- Slimfast shake
- Low-fat natural or plain yoghurt drinks
- Complan soup
- Meritene soup
- Protein Water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Fluids to avoid:
- Fruit juices, malt drinks and fruit smoothie’s with bits
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Sample meal plan
Breakfast: High protein shake
Lunch: Slimfast shake or Meritine/Complan soup (1 sachet)
Evening meal: High protein shake or Meritene/Complan Soup
Snacks in between meals: if you feel hungry in between meals you can consume 200ml of skimmed/semi-skimmed/lacto-free/soya milk with or without the addition of 1 tablespoon of skimmed milk powder.
Stage 2 – only puree foods for 1 week
All food during this stage should be pureed and completely smooth with no bits or lumps.
Puree foods are smooth and can pass through your stomach easily. You will need to use a blender, liquidiser or food processor to puree your food to the correct consistency. Aim for a smooth consistency like ‘yoghurt’.
Include foods that are high in protein in your meals to keep you fuller for longer, and also prevent muscle loss.
How much and when?
Eat 5-6 small meals throughout the day during this stage. Start with 1-2 tablespoons at your meals and snacks, and if you feel comfortable gradually increase the amount. As you progress through the puree stage, you may find that your portions gradually increase. However, remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
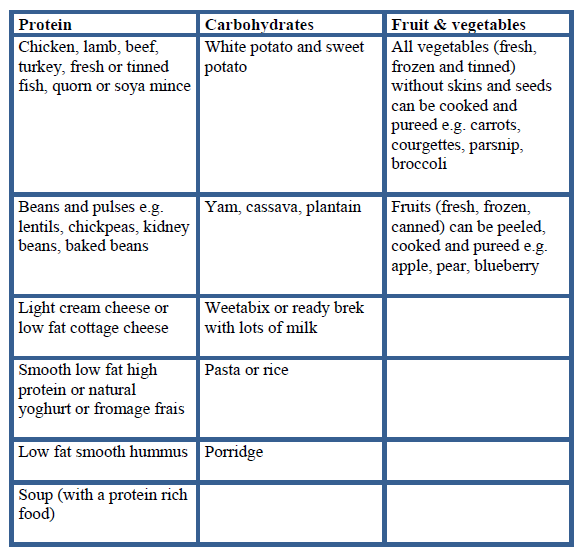
Which foods are suitable?
The main focus for your meals and snacks is protein so always eat this first. All of the foods in the table below will need to be pureed. Foods from other food groups such as carbohydrates, fruit and vegetables are also suitable, but are not a rich source of protein. If you choose to eat these then add some extra protein such as; protein or skimmed milk powder, high protein yoghurt, skimmed milk or low fat cheese to fortify them.
Foods to avoid:
Any food not pureed with a blender, liquidiser or food processor.
Suitable fluids:
- Skimmed/Semi-skimmed milk/Soya/Lacto-free milk
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
- Smooth fruit smoothies made with milk or skimmed milk powder.
Aim to drink 1.5-2 litres of fluids each day.
Fluids to avoid:
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Sample meal plan
Breakfast: Weetabix, Oatibix or Ready Brek with plenty of skimmed milk OR high protein yogurt pot or pouch
Lunch and Dinner ideas:
- Puree chicken with potato and vegetables
- Puree spaghetti bolognaise and vegetables
- Puree lentil or vegetable or chicken soup
- Puree tinned fish (tuna, sardines, mackerel) with potato and vegetables
Half your meal portion should be from a protein rich food. Try adding 2tsp of protein or skimmed milk powder to your puree foods.
Snacks: aim for 2-3 across the day: 200ml glass of skimmed milk (add 1-2tsp of skimmed milk powder) or protein shake or high protein yoghurt
Stage 3 – soft, fork-mashable foods for 2 weeks
Once you have completed the puree stage you can move onto soft foods. It is important to follow this stage as your stomach is still healing and recovering from surgery.
What is soft food?
Soft foods are foods that have a soft consistency, are well cooked and can be easily mashed with a fork. You do not need to use a blender during the soft stage.
Foods to avoid:
Any foods that are hard or contain skins, seeds and pips as these will be difficult to mash into a soft consistency
- Sweet corn, peas, celery, fresh tomato, potato skin, nuts, seeds, hard cheese
- Dry, crumbly foods e.g. biscuits, crackers
- Food that has a mixed consistency e.g. minestrone soup, cereal flakes with milk
How much and when?
Eat 3 meals each day and if you feel hungry between your meals, then have a snack. Use a side plate for your main meals, and fill ½ of your plate with protein rich foods. Start with 3-4tbsp at meal times and stop eating at the first signs of fullness or if you feel uncomfortable. Remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
What foods are suitable?
The main focus for your meals and snacks is protein, so continue to eat this first.
Sample meal plan
Breakfast ideas:
- Porridge, Oatibix or Weetabix with skimmed milk
- Mashed baked beans
- Soft cooked eggs e.g. scrambled, poached, omelette
Lunch and Dinner ideas:
- Tinned or soft flaky fish with mashed potato and vegetables
- Shepherd’s pie or cottage pie with mashed vegetables
- Minced chicken/beef/lamb/turkey with couscous/mashed potato and vegetables
- Minced quorn or soya mince with pasta and vegetable
- Omelette with low fat grated cheese with mashed, peeled, seedless tomato
- Cauliflower cheese
- Risotto with soft mashed vegetables
- Chicken or meat casserole
- Thick soups e.g. lentil, ham, leek and potato
Snack ideas:
- 200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder) or high protein yoghurt or low fat custard or low fat yoghurt
Suitable fluids:
- Skimmed/Semi-skimmed milk/Soya/Lacto-free milk
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
- Smooth fruit smoothies made with milk or skimmed milk powder.
Aim to drink 1.5-2 litres of fluids each day.
Fluids to avoid:
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Stage 4 – regular foods from week 5 onwards
From week 4 after surgery your stomach should have healed enough for you to gradually introduce regular texture foods and increase the variety of foods in your diet.
Continue to eat 3 regular meals each day and try not to leave more than 3-4 hours between meals. You should not graze (eat small amounts of food constantly through the day) or go for a long-period of time without eating.
Use a side plate to help guide your portions and follow the plate model below, so that you are always prioritising protein first. If you are hungry in-between meals then choose a nutritious snack such as a piece of fruit, high protein yoghurt or a glass of skimmed/semi skimmed milk.

EAT FIRST: Protein (meat, fish, poultry, eggs, beans, pulses)
EAT SECOND: Vegetables and salad
EAT LAST: Carbohydrates (bread, rice, potato, pasta, grains)
There may be foods after a gastric band insertion that some people find difficult to tolerate and feel like they get ‘stuck’ or may make you sick. These include; chewy or dry red and white meat, bread, fibrous fruit and vegetables, rice, pasta, nuts and seeds. Avoid these at the beginning of the regular stage (stage 4) and then re-introduce them gradually once a ‘regular’ diet has been established.
What shall I do if food gets stuck?
If this happens it may be because you have eaten a food that was too solid, eaten too quickly or too much, or because of eating certain ‘problem’ foods. This will feel uncomfortable and you may wretch or vomit. Often it will resolve itself, however you could try drinking a small amount of cold sparkling water, as the fizz may help to dislodge the food that is stuck.
What else can you expect after surgery?
Side effects
Vomiting
After your surgery vomiting can occur. It is often the result of:
- Eating too much
- Eating too quickly
- Not chewing your food well enough
- Eating and drinking together, or too closely together
- Eating foods that are not the correct consistency for the stage you are in
- If you continue to vomit after checking the above and you are still within the first 2 months after surgery, you could try returning to the puree or liquid phase for a short period to see if your symptoms improve.
- If you continue to vomit and the cause cannot be explained then please contact your surgeon or GP.
Constipation
You may experience constipation during texture progression stages due to reduced fibre intake. If you experience constipation make sure you are drinking enough fluids. You should aim for 1.5-2 litres of fluids each day. During the early post-operative stages it can be difficult to get enough fibre as your focus is on protein. When you are in the puree stage, include some puree cereals and fruit and vegetables in your diet to help your bowels work more efficiently. If constipation persists then speak to your GP about a suitable laxative.
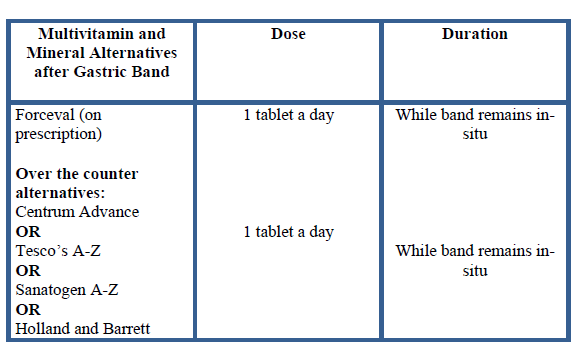
Vitamins and minerals
Due to the reduced portion sizes and overall food intake, you will not get adequate vitamins and minerals from the diet. Therefore you will need to start taking an additional vitamin and mineral supplementation once daily. As soon as you are able to start having liquids, you can begin taking your multivitamin and mineral supplement.
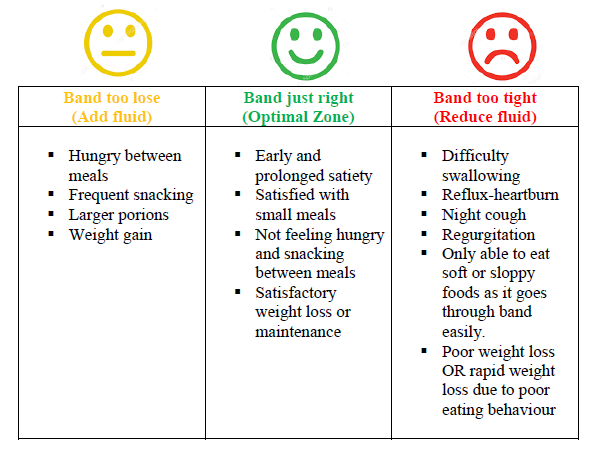
Gastric Band Adjustments:
Your first appointment for a gastric band adjustment will be 6-8 weeks following surgery. This fill is usually done under X-ray and the position of your band will also be checked at this time. Further band fills can be arranged through the bariatric nurse specialist in band clinic in outpatients or, under X-ray.
Prior to your first band fill you may start to feel hungry. This is because the band is usually empty and the swelling around the band from surgery that originally caused some feeling of restriction has reduced. It is very important that you follow the ‘golden rules’ (see the last page) and eat healthily to avoid weight gain prior to your first band fill.
There are some indications that show whether the band is too loose, too tight or band is just right. The table below shows these indications. Please be aware; if the band is too tight, you may either lose weight due to not being able to keep anything down or you may gain weight because you can only tolerate liquid or very sloppy foods which may be higher in calories.
Dietary goals for successful weight loss after bariatric surgery ‘The Golden Rules’
- Eat 3 small regular meals each day, avoid long periods of fasting
- Do not ‘graze’
- Plan snacks if you get hungry between meals
- Use a side plate to portion your meals
- Eat protein foods first
- Eat slowly: put a small amount of food in your mouth at a time (size of a thumbnail) and chew this very well (at least 20 times). Take 20-30 minutes to complete your meal
- Eat at a table or without any distractions and try putting your cutlery down between mouthfuls
- Do not eat until you are ‘full’. Overeating will stretch your stomach pouch, cause discomfort and may cause vomiting
- Do not drink with meals. Drink 20 minutes before meals and then wait at least 20 minutes after a meal before you drink some fluids
- Aim to drink at least 1.5-2 litres of fluid a day
- Avoid all alcohol
- Avoid all fizzy drinks as these can cause discomfort, bloating and stretch your small stomach pouch
- Avoid high calorie drinks such as smoothies, fruit juice, energy drinks and milkshakes as they contain a lot of sugar (and therefore calories) and can affect your weight loss following surgery

