Radiofrequency Induced Thermo-Chemotherapy with Mitomycin C / Epirubicin
This leaflet contains evidence-based information about Hyperthermic Mitomycin. We have consulted specialist surgeons during its preparation, so that it represents best practice in UK urology.
This leaflet contains evidence-based information about Hyperthermic Mitomycin. We have consulted specialist surgeons during its preparation, so that it represents best practice in UK urology.
|
Key Points
|
What does this procedure involve?
Instillation of an anti-cancer drug (usually Mitomycin C or Epirubicin) into your bladder, through a catheter (pictured on page 3), for aggressive, multiple or recurrent non-muscle invasive cancer of the bladder.
What are the alternatives?
- Repeated cystoscopy – with biopsy and electrical or laser cauterisation of any tumours found
- Intravesical immunotherapy – instillation of BCG (an inactivated strain of tuberculosis bacteria) into the bladder
- Surgical removal of the bladder (radical cystectomy) - with urinary diversion or bladder reconstruction
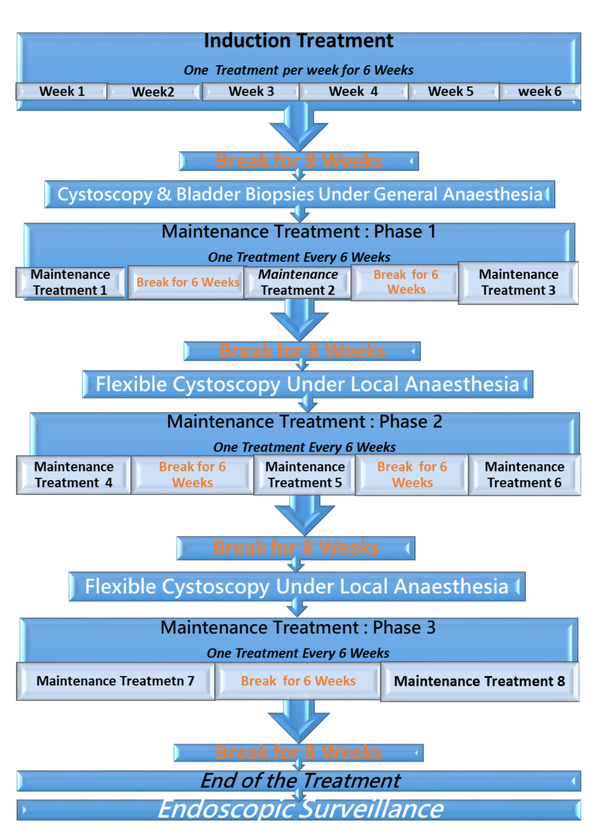
Treatment Schedule: Hyperthermic Mitomycin / Epirubicin
What happens on the day of the procedure?
You do not need to fast, you can eat and drink as usual; however, do not drink excessive fluids, specifically tea and coffee on the day of the procedure.
On arrival in the clinic, you will be asked to pass urine which we will test for infection. If an infection is suspected, we will send a sample to the laboratory and, depending on your symptoms, your procedure may be postponed whilst you take a course of antibiotics.
If you urine is clear, your urologist (or a member of their team) will briefly review your history and medications, and will discuss the procedure again with you to confirm your consent.
You should allow approximately 90 minutes for your first treatment.
Details of the procedure
- We clean your genital area with an antiseptic solution and squirt an antiseptic gel, containing local anaesthetic, into your urethra (waterpipe)
- We then pass a catheter into your bladder (pictured below) and we empty the bladder.
- We put 50 mls of the anti-cancer drug (normally
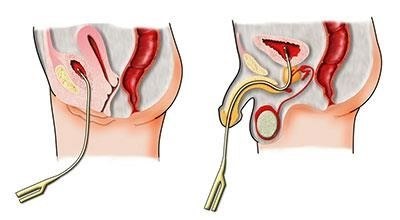
Mitomycin C or Epirubicin) into your bladder through the catheter
- The catheter is than connected to the Synergo system.
- The radiofrequency antenna embedded in the catheter will heat the bladder walls.
- The drug within the bladder constantly circulates between the bladder and the cooling chamber of the Synergo system.
- Upon completion of 30 minutes, the drug is removed from the bladder and a newly formulated drug (50 mls of Mitomycin C or Epirubicin) is injected into the bladder via the catheter.
- The bladder walls are heated with and the fluid in the bladder is cooled for another 30 minutes.
- Upon completion of the treatment, the bladder is emptied and the catheter is removed.
- on your first visit, we normally keep you in the clinic until you have passed urine but, for any remaining treatments, you can normally leave after one hour and pass urine at home
- there is no risk of contamination with the anti-cancer drug when you get home
- you should drink plenty of fluids (two to three litres) for the first few days after the treatment
- we usually repeat the procedure every week for 6 weeks; the urology staff will advise you about the need for any further, maintenance treatments
Are there any after-effects?
The possible after-effects and your risk of getting them are shown below.
Some are self-limiting or reversible, but others are not. We have not listed very rare after-effects (occurring in less than 1 in 250 patients) individually. The impact of these after-effects can vary a lot from patient to patient; you should ask your surgeon’s advice about the risks and their impact on you as an individual:
| After-effect | Risk |
| Some degree of bladder discomfort during the treatment | Between 1 in 2 & 1 in 10 patients |
| Irritation at the tip of urethra on passing urine | Between 1 in 2 & 1 in 10 patients |
| Discolouration of your urine | Between 1 in 2 & 1 in 10 patients |
| Blood in your urine | Between 1 in 2 & 1 in 10 patients |
| Debris in your urine | Between 1 in 2 & 1 in 10 patients |
| A skin rash | Between 1 in 10 & 1 in 50 patients |
| Failure to complete the course of treatment because of bladder discomfort | Between 1 in 10 & 1 in 50 patients |
| Infection in your urine | Between 1 in 10 & 1 in 50 patients |
| Stricture (narrowing) of the urethra (water pipe) following repeated use of a catheter | Between 1 in 10 & 1 in 50 patients |
| Severe pain on instillation which persists after you have emptied your bladder | Between 1 in 50 & 1 in 250 patients |
| An allergic reaction to the instilled drug, resulting in you having to stop the treatment | Between 1 in 50 & 1 in 250 patients |
| Long-term shrinkage of the bladder with a reduction in your bladder capacity | Between 1 in 50 & 1 in 250 patients |
What can I expect when I get home?
- a copy of your treatment details will be sent to your GP
- any antibiotics or other tablets you may need will be arranged & dispensed, either from the hospital pharmacy or by your GP
- you should always wash your hands and genitals every time you pass urine over the next few days (we also suggest that you bring a washbag with you every time you come to the hospital for treatment)
- you should not have sex for at least 24 hours after the treatment, because you may find it quite uncomfortable
- there is no risk of contamination with the drug when you get home
- if you are a smoker, you should try to stop because smoking can encourage the return of bladder cancer (see below)
General information about surgical procedures
Before your procedure
Please tell a member of the medical team if you have:
- an implanted foreign body (stent, joint replacement, pacemaker, heart valve, blood vessel graft);
- a regular prescription for a blood thinning agent (e.g. warfarin, aspirin, clopidogrel, rivaroxaban, dabigatran);
- a present or previous MRSA infection; or
- a high risk of variant-CJD (e.g. if you have had a corneal transplant, a neurosurgical dural transplant or human growth hormone treatment).
Questions you may wish to ask
If you wish to learn more about what will happen, you can find a list of suggested questions called "Having An Operation" on the website of the Royal College of Surgeons of England. You may also wish to ask your surgeon for his/her personal results and experience with this procedure.
Before you go home
We will give you advice about what to look out for when you get home. Your surgeon or nurse will also give you details of who to contact, and how to contact them, in the event of problems.
Smoking and surgery
Since you are only having a local anaesthetic, stopping smoking will have no effect on this procedure. Smoking can, however, cause cancers of the urinary tract and cause existing cancers to recur or progress. We strongly advise anyone with bladder cancer to stop smoking. For advice on stopping, you can:
- contact your GP;
- access your local NHS Smoking Help Online; or
- ring the free NHS Smoking Helpline on 0300 123 1044.
Driving after any procedure
It is your responsibility to make sure you are fit to drive even after a minor surgical procedure. You only need to contact the DVLA if your ability to drive is likely to be affected for more than three months. If it is, you should check with your insurance company before driving again.
What should I do with this information?
Thank you for taking the trouble to read this information. Please let your urologist (or specialist nurse) know if you would like to have a copy for your own records.
What sources have we used to prepare this leaflet?
This leaflet uses information from consensus panels and other evidencebased sources including:
- the Department of Health (England);
- the Cochrane Collaboration; and
- the National Institute for Health and Care Excellence (NICE).
It also follows style guidelines from:
- the Royal National Institute for Blind People (RNIB);
- the Information Standard;
- the Patient Information Forum; and
- the Plain English Campaign.
Disclaimer
We have made every effort to give accurate information but there may still be errors or omissions in this leaflet.

