Clostridioides difficile (C. diff)
What is Clostridioides difficile (C. diff)?
Clostridioides difficile (C. diff) is a bacterium that can live naturally in the gut. It is present in small numbers in approximately 5% of healthy adults. It is kept in check by the normal ‘good’ bacterial population of the gut. C. diff is also common in the intestine of babies and infants but does not cause disease because its toxins do not damage their immature intestinal cells.
Some patients may develop C. diff when they take antibiotics for other bacterial infections. Antibiotics can disturb the balance of the good bacteria in the gut, allowing C. diff to grow and produce toxins that may damage the cells lining the bowel.
How is C. diff diagnosed?
C. diff is diagnosed by sending a stool sample to the laboratory to test for C. diff.
What are the symptoms of C. diff disease?
C. diff causes a range of symptoms from a very mild disturbance to severe disease. These symptoms may include diarrhoea, abdominal pain or tenderness, dehydration, nausea, loss of appetite, fever, colitis (ulceration and bleeding of the colon) or inflammation of the bowel.
Tell a member of staff urgently if you develop severe abdominal pain, blood in your stools, a high temperature or signs of dehydration (such as dizziness, a very dry mouth or passing very little urine).
How does it spread?
C. diff can be spread through spores. When someone has C. diff diarrhoea, the bacteria can form spores (bacteria with a protective coating) which are designed to survive outside the human body. These spores can contaminate the environment. Spores can survive for some time and can be a source of infection to others if the environment is not thoroughly cleaned.
C. diff can spread onto your hands if you have direct contact with someone who is infected or if you touch a contaminated surface. If you then eat or touch your mouth, you may swallow spores.
Will I need to be in isolation?
If you have diarrhoea in hospital, we may transfer you to a single room to prevent C. diff spreading to other patients. This is a normal infection prevention measure. You will be taken out of isolation when you are no longer having diarrhoea and are passing normal stools.
Preventing the spread of C. diff
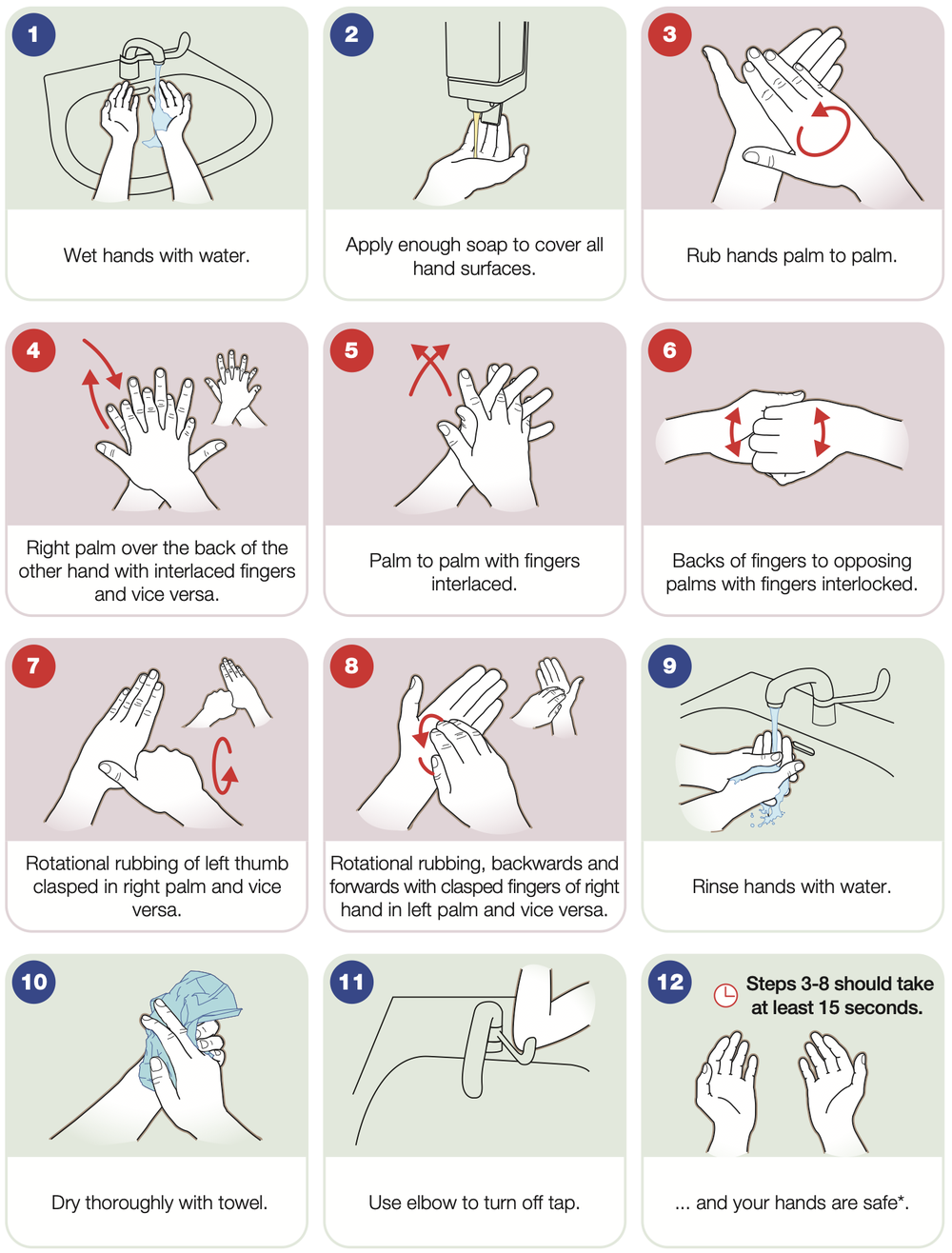
Hand hygiene is essential in preventing the spread of C. diff. Staff and visitors should always wash their hands with soap and water after coming into contact with patients or their surroundings. Alcohol-based hand rub is not effective against C. diff spores.
You should always wash your hands with soap and water after using the toilet and before eating. If you need help with this, ask staff on the ward.
The illustrations below show the technique that should be used.
Staff will wear gloves and aprons when caring for you. You will be allocated a toilet or commode for your use only. Cleaning of your room, toilets and other equipment is important and will be done regularly by the ward team.
Keep your bedside table or locker as clear as possible, to make it easy for staff to clean these surfaces regularly. Keep food in sealed containers and store them in your bedside locker rather than on your bedside table.
How is it treated?
It is generally treated for 10–14 days with a course of antibiotics that are taken orally. It is important that you complete the course of antibiotics even if your diarrhoea settles, otherwise symptoms may recur.
C. diff infections usually respond well to treatment, with most people making a full recovery in a week or two. If you have diarrhoea after stopping treatment, please tell your nurse, doctor or GP. As with any kind of diarrhoea, you are encouraged to drink plenty of fluids.
Can I have visitors in hospital or when I go home?
Yes, you can have visitors in hospital and at home. C. diff is unlikely to affect healthy relatives and friends. Your visitors should practise good hand hygiene by washing with soap and water before entering and leaving the bed space or isolation room, as described above.

