Chelsea Centre for Gender Surgery
Metoidioplasty Patient Information
Metoidioplasty Patient Information Leaflet Thank you for choosing the Chelsea Centre for Gender Surgery service at Chelsea and Westminster Hospital. We have worked with service specialists and the Transgender community to aim to deliver a high quality, patient centred service, with the aim of fully supporting you through your surgical journey. This leaflet will provide you with information about your Metoidioplasty surgery and what to expect before and after your operation.
Introduction
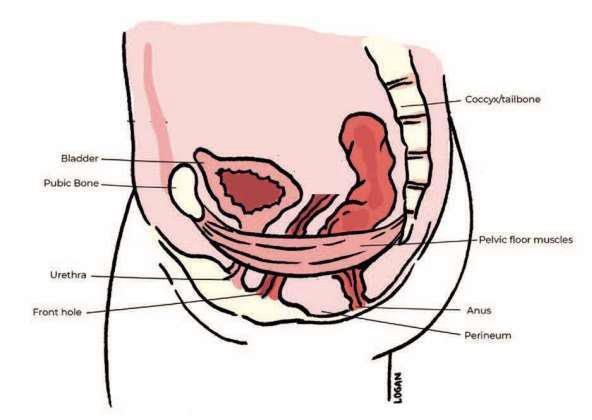
Metoidioplasty is a surgical procedure which creates a neo-phallus (small penis) from existing genital tissue. The clitoral tissue is detached from the labia and ligaments cut to form a masculine looking phallus, whilst retaining sensitivity. If you wish to pass urine through your neo-phallus, you can also have a urethroplasty (urethral lengthening plus connection (or hook-up) to the native water passage). The combination of the metoidioplasty and urethroplasty will allow you to urinate standing up. You are able to have the metoidioplasty element on its own, which would give you the neo-phallus, but allow you to keep your existing urethral opening. You would need to urinate sitting down in this instance. Urethral lengthening without hook-up is often offered if you don’t want to consider the full urethroplasty, with the purpose to obtain a wider girth of the neophallus—choosing this last option will allow you to potentially have the connection (hook-up) of the urethra done in a second stage.
The main intended benefit is the alleviation of gender dysphoria. Other benefits versus phalloplasty are that there will be no donor site scarring generally visible (only inside cheek potentially if a buccal mucosa graft is taken). The recovery time for a metoidioplasty is shorter compared to that of a phalloplasty.
Additional urethral reconstruction may be performed using tissue from the labia minora, or less frequently using a “buccal mucosa graft” (small flap of skin from the inner cheek). The buccal mucosa graft is harvested from the inner cheek. It is possible the addition of scrotal implants and/or retention of the vagina. While retaining sensitivity, it is a less effective surgical approach for patients wanting a phallus comparable in size to that of a cis male, or who wish to perform a penetrative role in sexual intercourse using their phallus.
We recommend reading through this leaflet carefully, noting down any questions you may have for your initial clinical nurse specialist and consultant surgeon appointments.
Pre-surgery appointments
Gender Affirmation Surgery (GAS) Clinical Nurse Specialist
Your first appointment will be an individualised consultation with a Clinical Nurse Specialist (CNS). This appointment is for you to ask any questions, hear more about the surgery and learn about the support that we can offer you as a team throughout your care. The nurse will ask questions about your medical history, some of which may be of a sensitive nature. They will also organise any tests that you require.
The option of fertility preservation (egg collection) will be discussed with you at your first nurse appointment if you have not already had a hysterectomy, or if you have had a hysterectomy but no salpingo-oophorectomy (removal of ovaries). Fertility preservation may be within the Imperial NHS trust or at an NHS trust that offers this service locally to you.
Your first appointment will be virtual, but future appointments will also be face-to-face. Please let us know at your initial appointment if you have difficulty attending appointments at the hospital in Chelsea.
For your first appointment please ensure you have:
- A written list of all your current medication, medical conditions and any operations or illnesses you have had
- Information from any other hospitals or doctors that you visit
- If you receive copies of hospital doctor's letters about you and your health, please bring them with you
First face-to-face appointment with your consultant surgeon
You will have an appointment with your consultant surgeon and this is an opportunity for you to ask any questions and discuss the surgery and what it entails and understand the outcomes of this surgery. The appointment will cover:
- Desired procedure detail, how long it will take, and what you should expect from this surgery
- A review of previous surgeries
- Initial Verbal informed consent discussion regarding the procedure, risks and outcomes
- Physical examination with the option of medical photography to be done on the day
- Advice about the use of vacuum pump device
In addition to your verbal consent conversation, you will receive a digital consent form which formally documents the discussion that you will have had with your consultant. The consent form will be sent to your email or mobile phone using our digital consent system known as Concentric. If you still need some more time after the first consultation, the form will be delayed and sent after the second encounter. This form confirms you are informed about the surgery including knowledge about the associated risks and complications of the procedure. You will need to sign this prior to your surgery.
Consent to the planned procedure will be confirmed with you again on the day of your surgery and any discussions or questions raised can be documented on your Concentric profile by the clinician.
Your consultant surgeon will discuss with you about when to stop your testosterone preoperatively.
If you have any difficulties with remotely consenting, please contact our Patient Pathway Co-ordinators. Their telephone contact details can be found on the last page of this information leaflet.
To make sure we provide you with the best possible holistic care your case will be discussed in the MDT (Multi-Disciplinary Team meeting) and the procedure can only go ahead with the agreement of the panel; sometimes further investigations/clinical steps are required before the MDT is happy for you to have the procedure.
Second surgical consultation
During this consultation (usually video or telephone based) we will discuss the outcome of the MDT, you will confirm the procedure you want to go ahead with and the consent discussion will also be retouched on. If not previously completed, the electronic consent form will be sent to you at this time. You will have all the time for reading it and signing it when you feel comfortable with the explanations.
When you attend for your consultant appointment you will also be seen by a specialist physiotherapist and your clinical nurse specialist who will be able to offer support and advice to you about your surgery.
Pre-operative assessment (usually six weeks before your operation)
You will attend a face-to-face appointment with a pre-operative nurse, who will talk through your previous and current medical history, arrange any tests such as blood tests that you need before surgery and give you information about preparing for your anaesthetic. We understand that you may need to travel a long distance to be seen in London, which is why, whenever it is appropriate, we may run the preoperative assessment during the same day of the face to face consultation, in the form of a one-stop clinic. If your pre-operative assessment has not been carried out on the day of the one-stop clinic a telephone assessment will be arranged and carried out with one of the pre-operative nurses, at least 6 weeks before your surgery.
Psychology support
Anxiety around surgery is normal and as a team we are here to support you; our clinical nurse specialists are available to answer any questions. We also have a psychologist who has specialist knowledge in trans healthcare who can support you pre or post operatively. People meet with our psychologists for all sorts of reasons including:
- To think about anxiety related to medical settings or procedures.
- Connect with their strengths and resources and plan what they might need at different times.
- To think about how they navigate surgery with the important people in their lives - for example how they share information or let them know what they need.
- To talk about experiences of transphobia and the effects this is having on them - for example, how they feel about themselves, others, or surgery.
- To think about how to understand anxiety or low mood, and how to respond to it, in relation to surgery or gender identity.
If you think it might be helpful to meet with our psychologist, just let your CNS know and they will arrange a referral.
Important points to note in the lead up to your surgery
- You will have to stop smoking for at least six weeks before your surgery date. If you require help with this, please speak to your clinical nurse specialist or access a stop smoking service near you.
- BMI/Weight loss—it is recommended for your BMI (Body Mass Index) to be 30 or less for the operation to achieve the best outcome. Additionally, there can be a higher risk of surgical and anaesthetic complications if you have a BMI over 30. This is something that can be discussed at your first appointment with your Clinical Nurse Specialist. Support and advice can be offered if you need to lose weight preoperatively.
- When you are provided with your surgery date we suggest letting your workplace know. Your fit note will be provided to you after surgery and will cover the period from your surgery date to when the surgeon deems you are ready to go back to work. This is normally at least three weeks post operatively depending on your type of work.
- You should continue to take all your regular medication on the morning of your operation as well as post-operatively, unless you have specifically been told not to. This will have been discussed with you in the pre-assessment clinic or by your surgeon. Taking medication that you have been asked not to or that has not been prescribed, may result in your operation being cancelled. Please bring all your medications into the hospital with you on the day of surgery.
Prior to surgery
We will ask you to carry out a routine Sexual Health Screen. This can be carried out when you attend your face-to-face consultations. If you develop or experience any symptoms, we advise you to visit your local sexual health services and to inform us of this.
One week before surgery
- It is required that you stop drinking alcohol one week before and for three weeks after surgery, because alcohol increases chances of bleeding—if you need support with this, let your Clinical Nurse Specialist know
- NO aspirin or any blood thinning medication
- NO nonsteroidal anti-inflammatory drugs- such as Ibuprofen, Diclofenac, or Naproxen
- NO herbal supplements eg St Johns Wort
- NO fish oil
- Wash and change bed sheets, as this will be more difficult to do when you get back from the hospital
- If you have had diarrhoea or vomiting 72 hours or less, before your operation, please contact the team as soon as possible, as your procedure will need to be rescheduled. It is also important that you inform us if you are feeling unwell, have had a temperature or flu like symptoms on or on the days leading up to your planned operation. It may be safer to postpone your operation until you are well.
- Please remove any nail varnish before you come in for your operation as it can interfere with monitoring.
Suggestions of things to stock up with at home
- Paracetamol for pain relief
- Easy to eat foods or ready meals
- High-fibre fruits, vegetables, pulses, and whole grains, which will help prevent constipation after a general anaesthetic
- A thermometer
- Anti-bacterial hand wash and gel
Day before admission
- Bowel preparation—for selected cases you may be given an oral medication at your pre op assessment to take the day before your surgery to ensure your bowels are emptied prior. Specific instructions will be given to you at your Pre-op appointment.
Suggestions of what to pack
- Clean and loose clothing such as jogging or pyjama bottoms—things that are easy to put on and take off
- A pillow for your own comfort
- Ear plugs and eye mask in case you have trouble sleeping in a hospital ward
- Reading material
- Toiletries
- Phone charger
- All medications that you are currently taking
- We recommend that you leave your jewellery at home
Day of surgery
Fasting instructions
- Morning Surgery: You can eat until midnight the night before the surgery you may drink sips of clear fluids (which includes only water, black tea, or black coffee until time of surgery)
- Afternoon Surgery: You must finish eating breakfast by 7am on the day of the surgery.
You may drink sips of clear fluids (which includes only water, black tea, or black coffee until time of surgery).
Why is fasting important?
Fasting (not eating, sips of clear fluids are allowed) is important to avoid complications with your anaesthetic during your operation.
What to expect on the day
It is important you arrive on time. Please note the time provided on your admission letter is not the time of your surgery. All patients for the morning or afternoon theatre list are asked to come in at the same time in order for us to run the list most efficiently. You may be waiting for a few hours for your surgery.
Arrival at the Surgical Admissions Lounge
When you arrive at the Surgical Admissions Lounge (SAL), you will be seen by a nurse or Healthcare Assistant (HCA) who will check your details, check your observations (pulse, blood pressure, temperature, height, and weight). You will also be provided with surgical compression stockings and a theatre gown to wear. The gown should be put on back-to-front, so it opens at the back. You may be able to leave your underwear on, until you are ready to go to theatre. Your nurse will let you know when you need to remove them before surgery.
On admission, all patients with a uterus will need to have a pregnancy test done.
Your anaesthetist and surgeon will also see you before your operation. The anaesthetist will discuss the anaesthetic plan, including providing you with information on how you can control your pain after the operation. Your surgeon will discuss the details of their plan, review the details of your consent form, and confirm you are happy to proceed. If required, they will mark the site of surgery.
When it is time for your surgery, a porter will take you from the Surgical Admissions Lounge to the Operating theatre.
Postoperative care
You will wake up from your surgery in the post-operative recovery area with one or two nurses monitoring your recovery post-surgery. Once they are happy with your status, you will be transferred to your elective surgical ward.
You will have dressings and surgical drains (although the latter will depend on the details of your operation) in situ around the wound site to help drain fluid to aid healing. These will remain in place for 1–2 days after your operation. A coban bandage will also be placed around the wound, as it is a durable, elastic wrap which will secure the dressing. It is important to note that this could look very similar to your skin. This will be stitched on which will mean that suture removal will also be undertaken at your first post op appointment. Please take simple analgesia such as paracetamol and/or ibruprofen (if you are able to do so) before your first post op appointment.
You will also have pad/gauze and mefix dressings immediately post op that will be removed on the ward round the following morning.
If you have full urethroplasty (urethral lengthening with hook-up) you will also have two urinary catheters—a catheter is a hollow, flexible tube designed to drain urine from your bladder. You will have a urethral catheter placed through your neo phallus and a suprapubic catheter inserted into the bladder through a tract made in the stomach wall.
If you have metoidioplasty without urethral lengthening OR with urethral lengthening but without hook-up, you will only have a single catheter passing through the normal water passage, which will usually be removed within 7 days. You may also have a little circular tube (splint) that will also remain in place until the first postoperative appointment (7–10 day post-op).
You will have a cannula which is most likely to be placed in your arm or hand, which will allow us to administer fluids and pain relief intravenously. If you are in pain or discomfort, let the nursing team know as soon as possible.
You will be able to eat and drink as normal after the operation. If you have had a buccal graft taken from the inside of your mouth to create your neourethra, your mouth may feel sore. You will be provided with mouthwash, and we recommend that you use this as prescribed.
You will be seen post operatively by a physiotherapist who will help you to mobilise out of bed after your surgery and give you advice for physical activity for when your return home and about pelvic floor health.
You will receive pain medication and antibiotics to go home with, all medications will be discussed with you on discharge and advice will be given to you on when to restart your testosterone.
Visitors while in hospital
The surgical theatres unit (where the operating theatres are located) are only for staff and patients undergoing their procedure. Relatives and/or friends are not permitted in this area. This includes the recovery area.
Once patients have been discharged from the recovery area to the surgical ward, they are allowed visitors (1–2 at a time). The ward will have specific allocated visiting hours, this can be confirmed with you Clinical Nurse Specialist before admission. Please note that the number of visitors and visiting times may vary in accordance with NHS Guidelines and the Trust’s visiting policy. The measures are put in place to protect our patients and staff when necessary. Changes or updates are available on the Trust website.
If you have special needs and require a carer to be with you; please speak to your Clinical Nurse Specialist prior to the day of surgery. A plan can be implemented before your admission to hospital.
Discharge information and aftercare
You will need to stay in hospital until your medical team decides it is safe for you to be discharged. The usual length of stay for metoidioplasty is 1–2 days.
It is required that if you live outside of London that you stay in London or within 60 minutes travel from the hospital, for at least 7–10 days after you have been discharged (more detail will be provided to you at your first CNS appointment).
You will also be able to shower, however it is important that you avoid soaking the coban bandage. Once showering, the wound area can also be gently dried by patting with a clean towel or using the cool setting on a hairdryer.
7–10 days after your operation
You will have an outpatient appointment with your Gender Affirmation Surgery Clinical Nurse Specialist who will review your general recovery. Your urethral catheter will be removed. If you chose not to have a full urethroplasty we will then make sure that you pass good amount of urine. If you chose to have a full urethroplasty, you will then use the suprapubic catheter to pass urine until its removal at day 21. At this appointment you will also be seen by the Plastics Nurse Specialists who will assess your wound healing, remove stiches and give you wound care advice for when you go home. It is also normal to have some localised swelling, mild post op bleeding and/or serous ooze from wounds. Patients are also asked to provide images of their wound healing via a safe and confidential programme known as ISLA. Pictures will also be taken by the nurses during your wound check appointment via ISLA to upload to your medical records.
21 days post-op
In case you opted for full urethroplasty (urethral lengthening plus hook up to native urethra) you will need to have your suprapubic catheter removed—this will be arranged for you by your Clinical Nurse Specialist at your local hospital or with the community team where you live or at Chelsea and Westminster Hospital.
Aftercare planning and recovery
- It is advisable to have a comfortable place to recover for 4 weeks post-surgery.
- We recommend that you have someone who can accompany you on discharge, come with you to your post-operative appointments and help with shopping, prepare meals, and make pharmacy visits.
- If you have chosen to have testicular implants inserted, you will need to be very careful in moving for the first week, limiting the amount of steps to 200 a day, and avoiding any trauma or compression to the area. Pain and bruising are expected.
- Some postoperative pain is always expected, but this should be manageable with the advices given to you at the discharge. Should this not be the case, please contact your GP or our team to discuss further options.
- It is possible to return to work once your suprapubic catheter is removed (21 days post operatively) depending on your job and the manual labour involved. Please discuss this with the team if you are unsure.
- We recommend that you do not do excessive or strenuous exercise for 2 months after your operation.
- Usually, it is recommended to wait at least 4 weeks post-surgery prior to engaging in sexual activity to allow time for the healing process. If you have any doubts regarding this, please ask your surgeon or specialist nurse.
If there are any clinical issues, do not wait until your next appointment. Please contact your Clinical Nurse Specialist to discuss.
Contact details
Please contact our Clinical Nurse Specialist Team if you have any questions about your care or surgery. They will provide their contact number to you directly at your first attendance.
Please contact our Patient Pathway Coordinators if you any questions about appointments or date of surgery, you need information about your care and treatment in a different format (such as easy read, large print, braille, or audio) due to disability, impairment or sensory loss or you require this information leaflet in another language. The email address for contacting them is: chelwest.ccgs.admin@nhs.net
Patient Advice and Liaison Service (PALS)
If you have concerns or wish to give feedback about services, your care or treatment, you can contact the PALS office on the Ground Floor of the hospital just behind the main reception.
Alternatively, you can send us your comments or suggestions on one of our comment cards, available at the PALS office, or on our feedback form.
We value your opinion and invite you to provide us with feedback.
T: 020 3315 6727
E: cwpals@chelwest.nhs.uk
Weight Management Support (Gender Affirmation Surgery)
This leaflet provides guidance for individuals whose current weight may delay their surgical journey. It outlines how reducing weight can improve surgical outcomes and minimise complications.
If your current weight is preventing you from having surgery, reducing your weight can lower the risk of post-surgical complications and improve outcomes.
Below are free NHS services and community resources to help you start your weight-loss journey.
How to access NHS weight management services
- Speak to your GP – they can provide advice and refer you to local weight management programmes.
- Self-refer – check with your GP surgery or local Integrated Care Board (ICB): Find your ICB
- Explore online resources:
- NHS Better Health – free tools, tips and the NHS Weight Loss Plan app
- NHS Digital Weight Management Programme – a free 12-week online programme for eligible individuals
Please note: Waiting time for these services will vary locally.
Find local services across the UK
- Local authority services – many councils offer free or subsidised weight management programmes. Search for “weight management” on your council’s website.
- Community groups – join local weight loss groups or fitness programmes for extra support.
- NHS website search – use the NHS site to find services near you.
Tier 3 and Tier 4 services
Your GP can refer you if you meet the eligibility criteria:
Tier 3—specialist, non-surgical weight management
- For people who have not succeeded with diet, exercise, or behavioural support
- Delivered by a multidisciplinary team of doctors, dietitians, psychologists and activity specialists
Eligibility:
- BMI ≥ 40, or
- BMI ≥ 35 with health conditions such as type 2 diabetes or sleep apnoea
Tier 4—surgical weight management
-
Focuses on weight-loss surgery with pre- and post-operative support (dietary advice, psychological support, and physical activity coaching)
Eligibility:
- Completion of a Tier 3 programme, and
- BMI ≥ 40, or
- BMI ≥ 35 with associated health conditions
Trans and non-binary fitness and wellbeing resources
- Misfits – fitness classes for trans and non-binary people in London, Manchester, Bristol, Brighton, Edinburgh, Sheffield, Cardiff, Belfast and Warrington
- Trans-fitness – connects people to inclusive personal trainers, coaching and sports clubs.
- Spectra London – advocacy and signposting for trans and non-binary people facing barriers to healthcare, including weight management
- Gendered Intelligence – support line for those affected by waiting times for gender-affirming care, including surgery delays linked to weight management
- T: 0800 640 8046
- E: supportline@genderedintelligence.co.uk
- WhatsApp: 07592 650 496
- Support line info
- GIRES TranzWiki – directory of non-commercial groups and organisations supporting trans and gender diverse people
Combined gender-affirming hysterectomy with metoidioplasty
Who is this information for?
This information is for people having a hysterectomy at the same time as metoidioplasty. This leaflet is intended for trans men, non-binary and intersex people who have decided on hysterectomy (with or without removal of the Fallopian tubes and ovaries) at the time of metoidioplasty after discussion with their gender specialist and surgeon. This leaflet only outlines the details of your hysterectomy - a further leaflet is available with more information on metoidioplasty.
This leaflet uses “hysterectomy” generally to describe all procedures including removing the womb with or without removal of the ovaries and Fallopian tubes. More information on these choices is found below.
Content Warning: this document uses some anatomy/biological terms where it’s important to be precise.

Gender-affirming hysterectomy
You may have many reasons for choosing hysterectomy. Some may not be related to your transition. Some people have severe pelvic pain that medicines or hormone treatments have not fixed. Others have profound post-orgasm bleeding or pain. The same medical reasons for performing hysterectomy for a cis woman can also apply to anyone with a womb. It is important to talk through your reasons with your gender specialist and surgeon.
Hysterectomy operations offered at Chelsea and Westminster
We offer laparoscopic surgery (a minimally invasive keyhole approach) for almost all patients having gender-affirming hysterectomy. You’ll have either a robotic-assisted or a laparoscopic hysterectomy or sometimes a vaginal hysterectomy.
With the robotic or laparoscopic types of hysterectomies, your surgeon will make several small incisions (surgical cuts) on your abdomen. They’ll put a laparoscope (a long, thin surgical tool with a video camera) through one of the incisions into your abdomen. The laparoscope lets your surgeon see the inside of your abdomen.
Carbon dioxide gas will be pumped into your abdomen to make space. This gives your surgeon more room to do your surgery. Your surgeon will also put long, skinny surgical tools into the other incisions on your abdomen.
- With a laparoscopic hysterectomy, your surgeon directly controls the surgical tools with their hands. They can see the images from the laparoscope on a television monitor.
- With a robotic-assisted hysterectomy, your surgeon sits at a console and controls a robot that moves the surgical tools. The console has a special monitor where they can see the images from the laparoscope on a high-definition 3D screen.
With both types of hysterectomy, your surgeon will remove your uterus, cervix and fallopian tubes through your front-hole, if possible. If you have decided on having one or both ovaries removed, your surgeon will also remove these. If your uterus or cervix (+/- ovaries) can’t be removed through your front-hole (for example if your uterus is enlarged by fibroids or you have a big ovarian cyst), your surgeon will make one of your abdominal incisions bigger and remove your uterus and cervix from there. This is uncommon. Then they’ll close your incisions with sutures (stitches). Prior to surgery, your wishes for specific bottom surgery will be discussed so the incisions do not interfere with the next steps of the operation.
What are the risks of surgery?
Robotic-assisted and laparoscopic hysterectomy are safe procedures and we have a low complication rate, but they remain major surgeries. Any surgery has the risk of complications – rarely these complications can be very serious. It’s important you understand these risks before you consent to surgery.
Immediate risks—during or shortly after surgery
Less common—fewer than 1 in 20:
- Conversion to subtotal hysterectomy (this is rare in our practice)
- Change from keyhole to open surgery if there are unexpected complications or the uterus is very large
- Significant bleeding requiring blood transfusion
Rare—fewer than 1 in 100:
- Compression injury to nerves around where we operate
- Damage to surrounding structures (like bowel, bladder, the ureters or blood vessels)
- Failure to complete procedure
- Perioperative risks of the anaesthetic and other medicines
Early risks—in the days after surgery
Common—more than 1 in 20:
- Abdominal and shoulder tip discomfort due to trapped gas
- Ileus (sluggish bowels)
- Pelvic infection requiring antibiotics
- Vaginal bleeding
- Wound complications
Less common—fewer than 1 in 20:
- Urinary retention (difficulty passing urine such that we need to place a urine catheter into your bladder for a short period of time)
Rare—fewer than 1 in 100:
- Blood clots (deep vein thrombosis or pulmonary embolus)
- Vaginal vault dehiscence (where the top of the front-hole comes open if the stitches fail. Sometimes this requires repair under general anaesthetic.)
- Need to go back into theatre
- Pelvic abscess, a 1 in 500 chance
- Vaginal vault haematoma (collection of blood at the top of the front-hole)
- Death, a 1 in 3,000 chance
Late risks—in the months or years after surgery
Common—more than 1 in 20:
- Infertility (if the uterus is removed, you will not be able to get pregnant. If both ovaries are removed, you will not subsequently be able to use your own eggs in assisted conception to have a baby unless you have previously undergone egg retrieval)
- Dyspareunia (discomfort during front-hole sex if you have decided to keep)
- Premature ovarian insufficiency/menopause symptoms (this is uncommon for patients taking long term testosterone but there is little evidence on long-term outcomes)
- Symptomatic abdominal adhesions (scar tissue forming after surgery)
Less common—fewer than 1 in 20:
- Hernia from a keyhole cut (port-site)
- Regret (the feeling of regretting having had gender affirming hysterectomy is poorly understood in the medical literature)
- Vaginal vault prolapse (where the top of the front-hole prolapses down into the front-hole, sometimes bulging out if you haven’t had a vaginectomy (removal of the vagina/front hole) at time of metoidioplasty)
What to expect
On the day of surgery
Most people are admitted to hospital on the day of their surgery. You will be admitted to an all-gender mixed-specialty surgical admissions area on the day of your operation and seen by the nurse. Your vital signs will be measured, and the nurse will run through a checklist of questions. Your surgeons will see you and go through the consent form you signed electronically. You will be seen by a few surgeons from the different specialties as part of gender affirmation surgery team, please do not be alarmed, you will already have met the majority of the team at your initial consultations. Ask any questions you have about your surgery, as we want you to be fully informed and involved in your care.
Depending on the order of the day’s operations, you may have to wait for a few hours to be brought to the operating theatre to start your surgery, so bring a book or tablet with you to keep you occupied. Free WiFi is available throughout the Trust premises.

After surgery
You will wake up initially after surgery has finished in the Recovery Room where a nurse will monitor you closely until you are fit to go back to the ward. You’ll go back to a male ward with single gender (male) shared bathrooms, or private en-suite facilities.
You will have a catheter (tube) in your bladder to allow drainage of your urine and you will go home with this. You may have a second catheter but more about this is explained in the metoidioplasty leaflet. This is usually removed between day 7 and 21 by a member of our team depending on the specific steps of the procedure you have opted for.
You will stay in hospital for a minimum of two days after your surgery. The day after surgery you will be reviewed by members of the whole team, you will be given further advice on moving around the ward and the maximum number of steps per day. It is important to move around the ward to help aid your recovery, reduce the risk of blood clots and getting you back to normal. Start by sitting up in bed and moving around on the bed. Then sit on the edge of the bed. When you feel able to do so safely, slowly stand up and start moving around. Have a light breakfast and drink lots of fluids. If you’re in pain, ask your nurse for more painkillers.
Surgical incisions
You will have between two and five small incisions on different parts of your abdomen. Each incision will be between 0.5 cm and 1 cm long. Stitches and/or surgical glue are used to close these surgical incisions, and any stitches used do not require removal and will slowly dissolve. Your surgical incisions may initially be covered with a dressing. You should be able to take this off about 24 hours after your operation and have a wash or shower (see section on washing and showering). Any stitches in your front-hole will not need to be removed, as they are dissolvable. If you have not opted for vaginectomy then you may notice a stitch, or part of a stitch, coming away after a few days or maybe after a few weeks. This is normal and nothing to worry about.
One of your small incisions will be in your belly button area, so it’s important that your belly button is very clean before you attend hospital for surgery. When taking a shower, use a cotton ear bud to gently clean the belly button with water and your normal soap or shower gel. You must shower the night before and the morning of surgery.
Standard laparoscopy incisions Robotic assisted incisions


Anaesthetic effects
Modern anaesthetics are short lasting. You should not have any after-effects for more than a day after your operation. During the first 24 hours you may feel more sleepy than usual and your judgement may be impaired. You are likely to be in hospital during the first 48 hours so by the time you have been discharged the anaesthetic will have fully worn off.
Bleeding
If you have not opted for vaginectomy you can expect to have some front-hole/vaginal bleeding for one to two weeks after your operation. This is like light menstrual bleeding and is red or brown in colour. Some people have little or no bleeding initially, and then have a sudden gush of old blood or fluid about 10 days later. This usually stops quickly. You should use sanitary towels rather than tampons as using tampons could increase the risk of infection.
Pain and discomfort
You can expect pain and discomfort in your lower abdomen and genital area for at least the first few days after your operation. You may also have some pain in your shoulder. This is a common side effect of laparoscopic surgery. It normally settles after 48 hours. When leaving hospital, you should be provided with painkillers for the pain you are experiencing. Sometimes painkillers that contain codeine or dihydrocodeine can make you sleepy, nauseated and constipated. If you do need to take these medications, try to eat extra fruit and fibre to reduce the chances of becoming constipated. Taking painkillers as prescribed to reduce your pain will enable you to get out of bed sooner, stand up straight and move around - all of which will speed up your recovery and help to prevent the formation of blood clots in your legs or your lungs.
Trapped wind
Following your operation your bowel may temporarily slow down, causing air or ‘wind’ to be trapped. This can cause some pain or discomfort until it is passed. Getting out of bed and walking around will help. Peppermint water may also ease your discomfort. Once your bowels start to move, the trapped wind will ease.
Starting to eat and drink
After your operation, you may have a drip in your arm to provide you with fluids. When you are able to drink again, and after any intravenous medications have been stopped, the drip will be removed. You will be offered a drink of water or cup of tea and something light to eat. If you are not hungry initially, you should drink fluid. Try eating something later on. Once you’ve passed wind after the operation, you can go back to a normal diet.
Washing and showering
You will not be able to bath, but you may shower, ensuring you do not scrub the area. If we have used dressings to cover your laparoscopy incisions for the hysterectomy part of the procedure these can come off after 2 days. If we have used glue this will dissolve on its own. You can get the glue and dressings wet but ensure you pat them dry. Keeping scars clean and dry helps healing. 7-10 days after your surgery your dressings in the genital area will be removed, but we do not recommend baths until all internal stitches have been dissolved, this is usually for at least 2 weeks.
Blood clots
There is a small risk of blood clots forming in the veins in your legs and pelvis (deep vein thrombosis) after any operation. These clots can travel to the lungs (pulmonary embolism), which could be serious.
You can reduce the risk of clots by:
- being as mobile as you can as early as you can after your operation
- doing exercises when you are resting, for example:
- pump each foot up and down briskly for 30 seconds by moving your ankle
- move each foot in a circular motion for 30 seconds
- bend and straighten your legs - one leg at a time, three times for each leg.
Most people will be given Clexane injections for ten days after your surgery to reduce the risk of blood clots forming. Your nurse will show you how to give yourself this injection when you go home. You’ll be given compression stockings (‘TEDS’) to wear during your stay in hospital.
Cervical smears
Most people can stop cervical smear tests after hysterectomy if your last cervical smear test was normal or you’ve never been sexually active before, or if we have performed a vaginectomy. If you have had abnormal smear tests before, discuss with your surgeon whether you should stop.
Hormones and T
Your surgeon will discuss with you before the surgery when to stop testosterone. If you’re taking topical estrogen in the front hole and have not had a vaginectomy (e.g. Vagifem or Ovestin) you can restart six weeks after surgery. If you’re taking other forms of HRT it’s important to discuss this with your surgeon at your initial consultation as you may need to stop.
Tiredness and feeling emotional
You may feel much more tired than usual after your operation as your body is using a lot of energy to heal itself. You may need to take a nap during the day for the first few days. A hysterectomy can also be emotionally stressful and many people feel tearful and emotional at first - when you are tired, these feelings can seem worse. For many people this is the last symptom to improve. If your mood is really affected, it’s important to seek help from friends, family or a medical professional.
What can help me recover?
Rest
Rest as much as you can for the first few days after you get home. It is important to relax, but avoid crossing your legs when you are lying down. Rest does not mean doing nothing at all throughout the day, as it is important to start exercising and doing light activities around the house within the first few days in line with your metoidioplasty leaflet guidance.
A pelvic floor muscle exercise programme
Separate leaflets are available on this subject. Please see POPG 'Fit following surgery’ and ‘Pelvic floor muscle exercises and advice’. These will be sent electronically to you along with your consent form.
A daily routine
Establish a daily routine and keep it up. For example, try to get up at your usual time, have a wash and get dressed, move about and so on. Sleeping in and staying in bed can make you feel depressed. Try to complete your routine and rest later if you need to.
Eat a healthy balanced diet
Ensure that your body has all the nutrients it needs by eating a healthy balanced diet. A healthy diet is a high-fibre diet (fruit, vegetables, wholegrain bread and cereal) with up to two litres per day of fluid intake, mainly water. Remember to eat at least five portions of fruit and vegetables each day! As long as you are exercising enough and don’t eat more than you need to, you don’t need to worry about gaining weight.
Keep your bowels working
Your bowels may take time to return to normal after your operation. Your motions should be soft and easy to pass. You may initially need to take laxatives to avoid straining and constipation. You may find it more comfortable to hold your abdomen (provide support) the first one or two times your bowels move.
If you do have problems opening your bowels, it may help to place a small footstool under your feet when you are sitting on the toilet so that your knees are higher than your hips. If possible, lean forward and rest your arms on top of your legs to avoid straining.
Stop smoking
Stopping smoking will benefit your health in all sorts of ways, such as lessening the risk of a wound infection or chest problems after your anaesthetic. By not smoking – even if it is just while you are recovering - you will bring immediate benefits to your health.
You will be required to stop smoking before your operation, remember to bring any nicotine replacement sprays or patches with you for use during your hospital stay. You will not be able to smoke in hospital. If you would like information about a smoking cessation clinic in your area, speak with the nurse in your GP surgery.
Support from your family and friends
You may be offered support from your family and friends in lots of different ways. It could be practical support with things such as shopping, housework or preparing meals. Most people are only too happy to help - even if it means you having to ask them! Having company when you are recovering gives you a chance to say how you are feeling after your operation and can help to lift your mood. If you live alone, plan in advance to have someone stay with you for the first few days when you are at home.
A positive outlook
Your attitude towards how you are recovering is an important factor in determining how your body heals and how you feel in yourself. You may want to use your recovery time as a chance to make some longer term positive lifestyle choices such as:
- starting to exercise regularly in line with our guidance if you are not doing so already and gradually building up the levels of exercise that you take
- eating a healthy diet - if you are overweight, it is best to eat healthily without trying to lose weight for the first couple of weeks after the operation; after that, you may want to lose weight by combining a healthy diet with exercise.
Whatever your situation and however you are feeling, try to continue to do the things that are helpful to your long-term recovery.
What can slow down my recovery?
It can take longer to recover from a hysterectomy if:
- you had health problems before your operation; for example, people with diabetes may heal more slowly and may be more prone to infection
- you smoke - smokers are at increased risk of getting a chest or wound infection during their recovery, and smoking can delay the healing process
- you were overweight at the time of your operation - if you are overweight, it can take longer to recover from the effects of the anaesthetic and there is a higher risk of complications such as infection and thrombosis
- there were any complications during your operation.
Recovering after an operation is a very personal experience. If you are following all the advice that you have been given but do not think that you are at the stage you ought to be, talk with your GP or one of our Clinical Nurse Specialists.
When should I seek medical advice after a hysterectomy as part of metoidioplasty?
While most people recover well after a laparoscopic hysterectomy and metoidioplasty, complications can occur - as with any operation. You should seek medical advice from your GP, the hospital where you had your operation, NHS 111 or NHS 24 if you experience:
- Burning and stinging when you pass urine or pass urine frequently when the catheter is out: This may be due to a urine infection. Treatment is with a course of antibiotics.
- Vaginal bleeding that becomes heavy or smelly if you haven’t had a vaginectomy: If you are also feeling unwell and have a temperature (fever), this may be due to an infection or a small collection of blood at the top of the front-hole called a vault haematoma. Treatment is usually with a course of antibiotics.
- Occasionally, you may need to be admitted to hospital for the antibiotics to be administered intravenously (into a vein). Rarely, this blood may need to be drained.
- Red and painful skin around your scars: This may be due to a wound infection. Treatment is with a course of antibiotics.
- Increasing abdominal pain: If you also have a temperature (fever), have lost your appetite and are vomiting, this may be due to damage to your bowel or bladder, in which case you will need to be admitted to hospital.
- A painful, red, swollen, hot leg or difficulty bearing weight on your legs: This may be due to a deep vein thrombosis (DVT). If you have shortness of breath or chest pain or cough up blood, it could be a sign that a blood clot has travelled to the lungs (pulmonary embolism). If you have these symptoms, you should seek medical help immediately.
- Further complications to be aware of are detailed in the metoidioplasty leaflet.
Getting back to normal
Around the house
While it is important to take enough rest, you should start some of your normal daily activities when you get home and build up slowly. You will find you are able to do more as the days and weeks pass. If you feel pain, you should try doing a little less for another few days.
It is helpful to break jobs up into smaller parts, such as ironing a couple of items of clothing at a time, and to take rests regularly. You can also try sitting down while preparing food or sorting laundry. For the first one to two weeks, you should restrict lifting to light loads such as a one litre bottle of water, kettles or small saucepans. You should not lift heavy objects such as full shopping bags or children, or do any strenuous housework such as vacuuming until three to four weeks after your operation as this may affect how you heal internally. Try getting down to your children rather than lifting them up to you. Remember to lift correctly by having your feet slightly apart, bending your knees, keeping your back straight and bracing (tightening or strengthening) your pelvic floor and stomach muscles as you lift. Hold the object close to you and lift by straightening your knees.
Exercise
While everyone will recover at a different rate, there is no reason why you should not start walking on the day you return home, specific number of steps are outlined in the metoidioplasty leaflet. You should be able to increase your activity levels slowly over the first few weeks.
Driving
You should not drive for 24 hours after a general anaesthetic. Each insurance company will have its own conditions for when you are insured to start driving again. Check your policy.
Before you recommence driving you should ensure that you are:
- able to make an emergency stop
- able to comfortably look over your shoulder to manoeuvre.
Before you drive you should be:
- free from the sedative effects of any painkillers
- able to sit in the car comfortably and work the controls
- able to wear the seatbelt comfortably
In general, it can take up to four weeks after metoidioplasty before you are able to do all of the above. It is a good idea to practise without the keys in the ignition. See whether you can do the movements you would need for an emergency stop and a three-point turn without causing yourself any discomfort or pain. When you are ready to start driving again, build up gradually, starting with a short journey.
Travel plans
If you are considering travelling during your recovery, it is helpful to think about:
- the length of your journey - journeys over four hours where you are not able to move around (in a car, coach, train or plane) can increase your risk of deep vein thrombosis (DVT);
- this is especially so if you are travelling soon after your operation
- how comfortable you will be during your journey, particularly if you are wearing a seatbelt
- regarding overseas travel:
- would you have access to appropriate medical advice at your destination if you were to have a problem after your operation?
- does your travel insurance cover any necessary medical treatment in the event of a problem after your operation?
- whether your plans are in line with the levels of activity recommended in this and the metoidioplasty information.
If you have concerns about your travel plans, it is important to discuss these with your GP or the hospital where you have your operation before travelling.
Having sex
You should usually allow six weeks after your operation to allow your scars to heal. It is then safe to have sex as long as you feel comfortable. If you have chosed to keep your front hole and you experience any discomfort or dryness you may wish to try a vaginal lubricant. You can buy this from your local pharmacy.
Returning to work
Everyone recovers at a different rate, so when you are ready to return to work will depend on the type of work you do, the number of hours and how you get to and from work.
You may experience more tiredness than normal after any operation, so your return to work should be like your return to physical activity, with a gradual increase in the hours and activities at work. If you have an occupational health department, they will advise on this.
Some people are fit to work after two to three weeks and will not be harmed by this if there are no complications from surgery. It may be better to wait for your day 21 review before returning to work.
Many people are able to go back to normal work after three to six weeks if they have been building up their levels of physical activity at home. Returning to work can help your recovery by getting you back into your normal routine again. Some people who are off work for longer periods start to feel isolated and depressed.
You do not have to be symptom free before you go back to work. It is normal to have some discomfort as you are adjusting to working life. It might be possible for you to return to work by doing shorter hours or lighter duties and build up gradually over a period of time.
Consider starting partway through your normal working week so you have a planned break quite soon. You might also wish to see your GP or your occupational health department before you go back and do certain jobs - discuss this with them before your operation. You should not feel pressured by family, friends, or your employer to return to work before you feel ready. You do not need your GP’s permission to go back to work. The decision is yours.

Gender-affirming hysterectomy
Who is this information for?
This information relates to planned gender-affirming hysterectomy as a standalone
procedure (ie it is not being undertaken at the same time as phalloplasty, metoidioplasty or other bottom surgeries). It should be noted that you may still have these surgeries separately after a standalone hysterectomy. This information is intended for trans men, non-binary and intersex people who have decided on hysterectomy (with or without removal of the fallopian tubes and ovaries) after discussion with their gender specialist and surgeon.
This leaflet uses “hysterectomy” generally to describe all procedures including removing the womb or uterus with or without removal of the ovaries and fallopian tubes. More information on these choices is found below.
Content warning: This document uses some anatomy/biological terms where it’s important to be precise.

Gender-affirming hysterectomy
You may have many reasons for choosing hysterectomy. Some may not be related to your transition. Some people have severe pelvic pain that medicines or hormone treatments have not fixed. Others have profound post-orgasm bleeding or pain. The same medical reasons for performing hysterectomy for a cis woman can also apply to anyone else with a womb. It is important to talk through your reasons with your gender specialist and surgeon.
Hysterectomy operations offered at Chelsea and Westminster
We offer laparoscopic surgery (a minimally invasive keyhole approach) for almost all patients having gender-affirming hysterectomy. You’ll have either a robotic-assisted or a laparoscopic hysterectomy or sometimes a vaginal hysterectomy.
With the robotic or laparoscopic types of hysterectomies, your surgeon will make several small incisions (surgical cuts) on your abdomen. They’ll put a laparoscope (a long, thin surgical tool with a video camera) through one of the incisions into your abdomen. The laparoscope lets your surgeon see the inside of your abdomen.
Carbon dioxide gas will be pumped into your abdomen to make space. This gives your surgeon more room to do your surgery. Your surgeon will also put long, skinny surgical tools into the other incisions on your abdomen.
- With a laparoscopic hysterectomy, your surgeon directly controls the surgical tools with their hands. They can see the images from the laparoscope on a television monitor.
- With a robotic-assisted hysterectomy, your surgeon sits at a console and controls a robot that moves the surgical tools. The console has a special monitor where they can see the images from the laparoscope on a high-definition 3D screen.
With both types of hysterectomy, your surgeon will remove your uterus, cervix and fallopian tubes through your front-hole, if possible. If you have decided on having one or both ovaries removed, your surgeon will also remove these. If your uterus or cervix (+/- ovaries) can’t be removed through your front-hole (for example if your uterus is enlarged by fibroids or you have a big ovarian cyst), your surgeon will make one of your abdominal incisions bigger and remove your uterus and cervix from there. This is uncommon. Then they’ll close your incisions with sutures (stitches). If you’re planning bottom surgery, it’s important your surgeon knows which bottom surgery you’re considering so that they can use an appropriate abdominal
incision in the unlikely event that open surgery is required.
What are the risks of surgery?
Robotic-assisted and laparoscopic hysterectomy are safe procedures, and we have a low complication rate, but they remain major surgeries. Any surgery has the risk of complications, and rarely these complications can be very serious. It’s important you understand these risks before you consent to surgery.
Immediate risks—during or shortly after surgery
Less common—fewer than 1 in 20:
- Conversion to subtotal hysterectomy (this is rare in our practice)
- Change from keyhole to open surgery if there are unexpected complications or the uterus is very large
- Significant bleeding requiring blood transfusion
Rare—fewer than 1 in 100:
- Compression injury to nerves around where we operate
- Damage to surrounding structures (like bowel, bladder, the ureters or blood vessels)
- Failure to complete procedure
- Perioperative risks of the anaesthetic and other medicines
Early risks—in the days after surgery
Common—more than 1 in 20:
- Abdominal and shoulder tip discomfort due to trapped gas
- Ileus (sluggish bowels)
- Pelvic infection requiring antibiotics
- Vaginal bleeding
- Wound complications
Less common—fewer than 1 in 20:
- Urinary retention (difficulty passing urine such that we need to place a urine catheter into your bladder for a short period of time)
Rare—fewer than 1 in 100:
- Blood clots (deep vein thrombosis or pulmonary embolus)
- Vaginal vault dehiscence (where the top of the front-hole comes open if the stitches fail. Sometimes this requires repair under general anaesthetic.)
- Need to go back into theatre
- Pelvic abscess, a 1 in 500 chance
- Vaginal vault haematoma (collection of blood at the top of the front-hole)
- Death, a 1 in 3,000 chance
Late risks—in the months or years after surgery
Common—more than 1 in 20:
- Infertility (if the uterus is removed, you will not be able to get pregnant. If both ovaries are removed, you will not subsequently be able to use your own eggs in assisted conception to have a baby unless you have previously undergone egg retrieval)
- Dyspareunia (discomfort during front-hole sex)
- Premature ovarian insufficiency/menopause symptoms (this is uncommon for patients taking long term testosterone but there is little evidence on long-term outcomes)
- Symptomatic abdominal adhesions
Less common—fewer than 1 in 20:
- Hernia from a keyhole cut (port-site)
- Regret (the feeling of regretting having had gender affirming hysterectomy is poorly understood in the medical literature)
- Front-hole vault prolapse (where the top of the front-hole prolapses down into the front-hole, sometimes bulging out)
What to expect
On the day of surgery
Most people are admitted to hospital on the day of their surgery and are discharged the same evening or the next morning. You will be admitted to an all-gender mixed-specialty surgical admissions area on the day of your operation and seen by the nurse. Your vital signs will be measured, and the nurse will run through a checklist of questions. Your surgeon or a member of their team will see you and go through the consent form you signed electronically. Ask any questions you have about your surgery, as we want you to be fully informed and involved in
your care.
Depending on the order of the day’s operations, you may have to wait for a few hours to be brought to the operating theatre to start your surgery, so bring a book or iPad with you to keep you occupied. Free NHS WiFi is available throughout the Trust premises.

After surgery
You will wake up initially after surgery has finished in the Recovery Room where a nurse will monitor you closely until you are fit to go back to the ward. You’ll go back to a male ward with single gender (male) shared bathrooms, or private en-suite facilities. If you would prefer to be accommodated after your operation on our dedicated female-only gynaecology ward, Annie Zunz, please let your surgeon know if this is the case during your first consultation or let the surgical scheduler know when you agree your date for surgery.
You may have a catheter (tube) in your bladder to allow drainage of your urine if your surgery is performed in the afternoon or your surgery took longer than average. This is usually removed the morning after surgery by a trained member of clinical staff familiar with transmasculine patients when you are easily able to walk to the toilet to empty your bladder. If you have problems passing urine, you may need to have a catheter for a few days to let the bladder rest before the catheter can be removed; this is uncommon.
If you’ve had a catheter inserted, you’ll probably stay overnight after your surgery. After your catheter is removed the morning after surgery, it’s important to move around early on to help your recovery. Start by sitting up in bed and moving around on the bed. Then sit on the edge of the bed. When you feel able to do so safely, slowly stand up and start moving around. Have a light breakfast and drink lots of fluids. If you’re in pain, ask your nurse for more painkillers.
Surgical incisions
You will have between two and five small incisions on different parts of your abdomen. Each incision will be between 0.5 cm and 1 cm long. Stitches and/or surgical glue are used to close these surgical incisions, and any stitches used do not require removal and will slowly dissolve. Your surgical incisions may initially be covered with a dressing. You should be able to take this off about 24 hours after your operation and have a wash or shower (see section on washing
and showering). Any stitches in your front-hole will not need to be removed, as they are dissolvable. You may notice a stitch, or part of a stitch, coming away after a few days or maybe after a few weeks. This is normal and nothing to worry about.
One of your small incisions will be in your belly button area, so it’s important that your belly button is very clean before you attend hospital for surgery. When taking a shower, use a cotton ear bud to gently clean the belly button with water and your normal soap or shower gel. You must shower the night before and the morning of surgery.
Standard laparoscopy incisions Robotic assisted incisions


Anaesthetic effects
Modern anaesthetics are short lasting. You should not have any after-effects for more than a day after your operation. During the first 24 hours you may feel more sleepy than usual and your judgement may be impaired. You are likely to be in hospital during the first 24 hours but, if not, you should have an adult with you during this time and you should not drive or make any important decisions.
Bleeding
You can expect to have some front-hole/vaginal bleeding for one to two weeks after your operation. This is like light menstrual bleeding and is red or brown in colour. Some people have little or no bleeding initially, and then have a sudden gush of old blood or fluid about 10 days later. This usually stops quickly. You should use sanitary towels rather than tampons as using tampons could increase the risk of infection.
Pain and discomfort
You can expect pain and discomfort in your lower abdomen for at least the first few days after your operation. You may also have some pain in your shoulder. This is a common side effect of laparoscopic surgery. It normally settles after 48 hours. When leaving hospital, you should be provided with painkillers for the pain you are experiencing. Sometimes painkillers that contain codeine or dihydrocodeine can make you sleepy, nauseated and constipated. If you do need to take these medications, try to eat extra fruit and fibre to reduce the chances of
becoming constipated. Taking painkillers as prescribed to reduce your pain will enable you to get out of bed sooner, stand up straight and move around - all of which will speed up your recovery and help to prevent the formation of blood clots in your legs or your lungs.
Trapped wind
Following your operation your bowel may temporarily slow down, causing air or ‘wind’ to be trapped. This can cause some pain or discomfort until it is passed. Getting out of bed and walking around will help. Peppermint water may also ease your discomfort. Once your bowels start to move, the trapped wind will ease.
Starting to eat and drink
After your operation, you may have a drip in your arm to provide you with fluids. When you are able to drink again, the drip will be removed. You will be offered a drink of water or cup of tea and something light to eat. If you are not hungry initially, you should drink fluid. Try eating something later on. Once you’ve passed wind after the operation, you can go back to a normal diet.
Washing and showering
You should be able to have a shower or bath and remove any dressings the morning after your operation. Don’t worry about getting your scars wet – just ensure that you pat them dry with clean disposable tissues or let them dry in the air. Keeping scars clean and dry helps healing.
Blood clots
There is a small risk of blood clots forming in the veins in your legs and pelvis (deep vein thrombosis) after any operation. These clots can travel to the lungs (pulmonary embolism), which could be serious.
You can reduce the risk of clots by:
- being as mobile as you can as early as you can after your operation
- doing exercises when you are resting, for example:
- pump each foot up and down briskly for 30 seconds by moving your ankle
- move each foot in a circular motion for 30 seconds
- bend and straighten your legs - one leg at a time, three times for each leg.
Most people will be given Clexane injections for ten days after your surgery to reduce the risk of blood clots forming. Your nurse will show you how to give yourself this injection when you go home. You’ll be given compression stockings (‘TEDS’) to wear during your stay in hospital.
Cervical smears
Most people can stop cervical smear tests after hysterectomy if your last cervical smear test was normal or you’ve never been sexually active before. If you have had abnormal smear tests before, discuss with your surgeon whether you should stop.
Hormones and T
You can continue your testosterone if you are taking it throughout the journey through surgery. If you’re taking topical estrogen in the front hole (e.g. Vagifem or Ovestin) you can restart six weeks after surgery. If you’re taking other forms of HRT except T it’s important to discuss this with your surgeon at your initial consultation as you may need to stop.
Tiredness and feeling emotional
You may feel much more tired than usual after your operation as your body is using a lot of energy to heal itself. You may need to take a nap during the day for the first few days. A hysterectomy can also be emotionally stressful and many people feel tearful and emotional at first - when you are tired, these feelings can seem worse. For many people this is the last symptom to improve. If your mood is really affected, it’s important to seek help from friends, family or a medical professional.
What can help me recover?
Rest
Rest as much as you can for the first few days after you get home. It is important to relax, but avoid crossing your legs for too long when you are lying down. Rest does not mean doing nothing at all throughout the day, as it is important to start exercising and doing light activities around the house within the first few days.
A pelvic floor muscle exercise programme
What are pelvic floor muscles?
Your pelvic floor muscles span the base of your pelvis. They work to keep your pelvic organs in the correct position (prevent prolapse), tightly close your bladder and bowel (stop urinary or anal incontinence) and improve sexual satisfaction if you use your front-hole. It is important for you to get these muscles working properly after your operation, even though you have internal stitches.
How to do pelvic floor exercises
To identify your pelvic floor muscles, imagine you are trying to stop yourself from passing wind, or you could think of yourself squeezing tightly inside your front-hole. When you do this you should feel your muscles ‘lift and squeeze’. It is important to breathe normally while you are doing pelvic floor muscle exercises. You may also feel some gentle tightening in your lower abdominal muscles. This is normal.
You can begin these exercises gently once your catheter has been removed (if present) and you are able to pass urine on your own. You need to practise short squeezes as well as long squeezes:
- short squeezes are when you tighten your pelvic floor muscles for one second, and then relax
- long squeezes are when you tighten your pelvic floor muscles, hold for several seconds, and then relax.
Start with what is comfortable and then gradually increase, aiming for 10 long squeezes, up to 10 seconds each, followed by 10 short squeezes. You should do pelvic floor muscle exercises at least three times a day. At first you may find it easier to do them when you are lying down or sitting. As your muscles improve, aim to do your exercises when you are standing up. It is very important to tighten your pelvic floor muscles before you do anything that may put them under pressure, such as lifting, coughing or sneezing.
Make these exercises part of your daily routine for the rest of your life. Some people use triggers to remind themselves such as, brushing their teeth, washing up or commercial breaks on television. Straining to empty your bowels (constipation) may also weaken your pelvic floor muscles and should be avoided. If you suffer from constipation or you find the pelvic floor muscle exercises difficult, you may benefit from seeing a specialist pelvic health physiotherapist.
A daily routine
Establish a daily routine and keep it up. For example, try to get up at your usual time, have a wash and get dressed, move about and so on. Sleeping in and staying in bed can make you feel depressed. Try to complete your routine and rest later if you need to.
Eat a healthy balanced diet
Ensure that your body has all the nutrients it needs by eating a healthy balanced diet. A healthy diet is a high-fibre diet (fruit, vegetables, wholegrain bread and cereal) with up to two litres per day of fluid intake, mainly water. Remember to eat at least five portions of fruit and vegetables each day! As long as you are exercising enough and don’t eat more than you need to, you don’t need to worry about gaining weight.
Keep your bowels working
Your bowels may take time to return to normal after your operation. Your motions should be soft and easy to pass. You may initially need to take laxatives to avoid straining and constipation. You may find it more comfortable to hold your abdomen (provide support) the first one or two times your bowels move.
If you do have problems opening your bowels, it may help to place a small footstool under your feet when you are sitting on the toilet so that your knees are higher than your hips. If possible, lean forward and rest your arms on top of your legs to avoid straining.
Stop smoking
Stopping smoking will benefit your health in all sorts of ways, such as lessening the risk of a wound infection or chest problems after your anaesthetic. By not smoking – even if it is just while you are recovering - you will bring immediate benefits to your health. If you are unable to stop smoking before your operation, you may need to bring nicotine replacements for use during your hospital stay. You will not be able to smoke in hospital. If you would like information about a smoking cessation clinic in your area, speak with the nurse in your GP surgery.
Support from your family and friends
You may be offered support from your family and friends in lots of different ways. It could be practical support with things such as shopping, housework or preparing meals. Most people are only too happy to help - even if it means you having to ask them! Having company when you are recovering gives you a chance to say how you are feeling after your operation and can help to lift your mood. If you live alone, plan in advance to have someone stay with you for the first few days when you are at home.
A positive outlook
Your attitude towards how you are recovering is an important factor in determining how your body heals and how you feel in yourself. You may want to use your recovery time as a chance to make some longer term positive lifestyle choices such as:
- starting to exercise regularly if you are not doing so already and gradually building up the levels of exercise that you take
- eating a healthy diet - if you are overweight, it is best to eat healthily without trying to lose weight for the first couple of weeks after the operation; after that, you may want to lose weight by combining a healthy diet with exercise.
Whatever your situation and however you are feeling, try to continue to do the things that are helpful to your long- term recovery.
What can slow down my recovery?
It can take longer to recover from a hysterectomy if:
- you had health problems before your operation; for example, people with diabetes
- may heal more slowly and may be more prone to infection
- you smoke - smokers are at increased risk of getting a chest
- or wound infection during their recovery, and smoking can delay the healing process
- you were overweight at the time of your operation - if you are overweight, it can take
- longer to recover from the effects of the anaesthetic and there is a higher risk of
- complications such as infection and thrombosis
- there were any complications during your operation.
Recovering after an operation is a very personal experience. If you are following all the advice that you have been given but do not think that you are at the stage you ought to be, talk with your GP.
When should I seek medical advice after a hysterectomy?
While most people recover well after a laparoscopic hysterectomy, complications can occur - as with any operation. You should seek medical advice from your GP, the hospital where you had your operation, NHS 111 or NHS 24 if you experience:
- Burning and stinging when you pass urine or pass urine frequently: This may be due to a urine infection. Treatment is with a course of antibiotics.
- Vaginal bleeding that becomes heavy or smelly: If you are also feeling unwell and have a temperature (fever), this may be due to an infection or a small collection of blood at the top of the front-hole called a vault haematoma. Treatment is usually with a course of antibiotics.
Occasionally, you may need to be admitted to hospital for the antibiotics to be administered intravenously (into a vein). Rarely, this blood may need to be drained.
- Red and painful skin around your scars: This may be due to a wound infection. Treatment is with a course of antibiotics.
- Increasing abdominal pain: If you also have a temperature (fever), have lost your appetite and are vomiting, this may be due to damage to your bowel or bladder, in which case you will need to be admitted to hospital.
- A painful, red, swollen, hot leg or difficulty bearing weight on your legs: This may be due to a deep vein thrombosis (DVT). If you have shortness of breath or chest pain or cough ,up blood, it could be a sign that a blood clot has travelled to the lungs (pulmonary embolism). If you have these symptoms, you should seek medical help Immediately
Getting back to normal
Around the house
While it is important to take enough rest, you should start some of your normal daily activities when you get home and build up slowly. You will find you are able to do more as the days and weeks pass. If you feel pain, you should try doing a little less for another few days.
It is helpful to break jobs up into smaller parts, such as ironing a couple of items of clothing at a time, and to take rests regularly. You can also try sitting down while preparing food or sorting laundry. For the first one to two weeks, you should restrict lifting to light loads such as a one litre bottle of water, kettles or small saucepans. You should not lift heavy objects such as full shopping bags or children, or do any strenuous housework such as vacuuming until three to four weeks after your operation as this may affect how you heal internally. Try getting down to your children rather than lifting them up to you. Remember to lift correctly
by having your feet slightly apart, bending your knees, keeping your back straight and bracing (tightening or strengthening) your pelvic floor and stomach muscles as you lift. Hold the object close to you and lift by straightening your knees.
Exercise
While everyone will recover at a different rate, there is no reason why you should not start walking on the day you return home. You should be able to increase your activity levels quite rapidly over the first few weeks. There is no evidence that normal physical activity levels are in any way harmful and a regular and gradual build-up of activity will assist your recovery. If you are unsure, start with short steady walks close to your home a couple of times a day for the first few days. When this is comfortable, you can gradually increase the time while walking at a relaxed steady pace. Many people should be able to walk for 30- 60 minutes after two or
three weeks. Swimming is an ideal exercise that can usually be resumed within two to three weeks provided that vaginal bleeding and discharge has stopped. If you build up gradually, the majority of people should be back to previous activity levels within four to six weeks. Contact sports and power sports should be avoided for at least six weeks, although this will depend on your level of fitness before surgery.
Driving
You should not drive for 24 hours after a general anaesthetic. Each insurance company will have its own conditions for when you are insured to start driving again. Check your policy.
Before you recommence driving you should ensure that you are:
- able to make an emergency stop
- able to comfortably look over your shoulder to manoeuvre.
Before you drive you should be:
- free from the sedative effects of any painkillers
- able to sit in the car comfortably and work the controls
- able to wear the seatbelt comfortably
In general, it can take two to four weeks before you are able to do all of the above. It is a good idea to practise without the keys in the ignition. See whether you can do the movements you would need for an emergency stop and a three-point turn without causing yourself any discomfort or pain. When you are ready to start driving again, build up gradually, starting with a short journey.
Travel plans
If you are considering travelling during your recovery, it is helpful to think about:
- the length of your journey - journeys over four hours where you are not able to move around (in a car, coach, train or plane) can increase your risk of deep vein thrombosis (DVT);
- this is especially so if you are travelling soon after your operation
- how comfortable you will be during your journey, particularly if you are wearing a seatbelt
- regarding overseas travel:
- would you have access to appropriate medical advice at your destination if you were to have a problem after your operation?
- does your travel insurance cover any necessary medical treatment in the event of a problem after your operation?
- whether your plans are in line with the levels of activity recommended in this information.
If you have concerns about your travel plans, it is important to discuss these with your GP or the hospital where you have your operation before travelling.
Having sex
You should usually allow four to six weeks after your operation to allow your scars to heal. It is then safe to have sex as long as you feel comfortable. If you experience any discomfort or dryness you may wish to try a vaginal lubricant. You can buy this from your local pharmacy.
Returning to work
Everyone recovers at a different rate, so when you are ready to return to work will depend on the type of work you do, the number of hours and how you get to and from work.
You may experience more tiredness than normal after any operation, so your return to work should be like your return to physical activity, with a gradual increase in the hours and activities at work. If you have an occupational health department, they will advise on this.
Some people are fit to work after two to three weeks and will not be harmed by this if there are no complications from surgery.
Many people are able to go back to normal work after three to six weeks if they have been building up their levels of physical activity at home. Returning to work can help your recovery by getting you back into your normal routine again. Some people who are off work for longer periods start to feel isolated and depressed.
You do not have to be symptom free before you go back to work. It is normal to have some discomfort as you are adjusting to working life. It might be possible for you to return to work by doing shorter hours or lighter duties and build up gradually over a period of time.
Consider starting partway through your normal working week so you have a planned break quite soon. You might also wish to see your GP or your occupational health department before you go back and do certain jobs - discuss this with them before your operation. You should not feel pressured by family, friends or your employer to return to work before you feel ready. You do not need your GP’s permission to go back to work. The decision is yours.

Your surgical plan
| Week before surgery | You may need to attend hospital for your pre-operative assessment and tests. You will be contacted if this is the case.
|
| Night before surgery |
|
| Morning of surgery |
|
| Immediately after surgery (in the recovery room) |
|
| Back on the ward (1–2 hours) |
|
| Back on the ward (2–4 hours) |
|
| Back on the ward (after 4 hours) |
|
Recovery tracker
| Time after operation | How might I feel? | What is safe to do? | Fit to work? |
| 1–2 days |
|
|
No |
| 3–7 days |
|
|
No |
| 1–2 weeks |
|
|
Maybe |
| 2–4 weeks |
|
|
Yes |
| 4–6 weeks |
|
|
Yes—if you do not feel ready to go back to work please discuss this with your GP |

