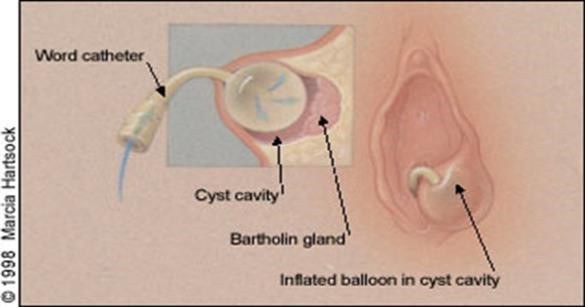
Word catheter for Bartholin’s abscess
This leaflet explains how inserting an inflatable balloon can be used to treat women with a Bartholin’s cyst or abscess. This leaflet is written to help women who have been offered this procedure to decide whether it is the right procedure for you.
What is a Bartholin’s abscess?
There is a Bartholin’s gland at each side of the entrance to the vagina. These glands produce lubrication that enters the vagina through a small duct (tube) from each gland. If the duct becomes blocked the gland can fill with mucus and a cyst (a fluid-filled lump) can occur. An abscess can occur if the gland or cyst becomes infected. Symptoms may include discomfort, tenderness/ pain, fever, and pain or discomfort during sex. A small procedure or surgical treatment may be used to drain it or to make a permanent opening that allows the gland to drain freely. Antibiotic treatment may have been initially used alone, but usually a persistent or growing abscess that is causing you symptoms also needs drainage.
Inflatable balloon insertion
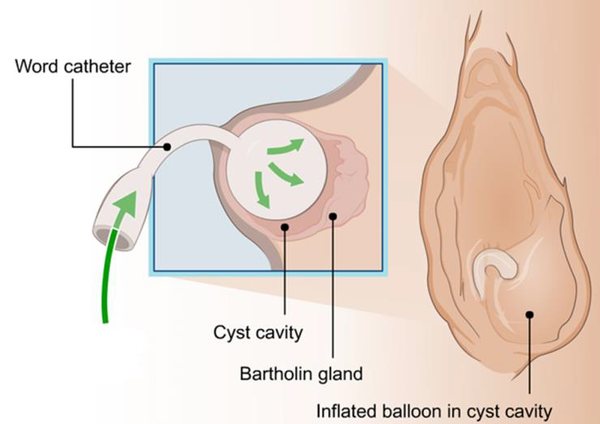
Insertion of an inflatable balloon is a non-surgical procedure that can be performed as an outpatient using a local anaesthetic (LA) injection to numb the area. It involves making a passage from the cyst or abscess through which the pus can drain over 4 weeks.

What are the advantages and disadvantages?
The advantages are that you do not need to be admitted to hospital, it avoids a general anaesthetic and is 97% successful. You can resume normal activities again once comfortable, including exercise. The catheter may cause minor discomfort but should not be painful. But avoid sex, tampons and swimming with the catheter in place.
Possible problems include pain if the balloon is too full, this can be relieved by removing some of the fluid. Occasionally the doctor or nurse will find that the abscess appears unusual or complex and therefore surgery is needed under general anaesthetic to treat it properly and a small sample of tissue (biopsy) is taken from the Bartholin’s gland for investigation. The Word catheter can be difficult to insert or cause an abscess, but this is uncommon.
Can this happen again?
Bartholin’s abscesses can occur again, whatever treatment is used (the long term recurrence rate is about 1 in 5, or 20%). With this inflatable balloon technique, the studies show a slightly lower rate of up to 17% recurrence over 4 years.)
Will I have any follow up?
After inserting a balloon catheter, the doctor or nurse will make a further appointment to see you again after 4 weeks, to deflate and remove the catheter. The cut in the skin heals over the next 5–7days. As mentioned, if the catheter is painful you should return to be examined and potentially removal of a small amount of the water in the balloon can provide relief.
Occasionally the catheter falls out before 4 weeks. If this occurs in the first 5 days, the doctor or nurse will try and reinsert it. If it is more than 5 days, then you will be advised to see what happens to the abscess; another catheter is only inserted if the abscess builds up again. Usually the organisms (‘bugs’) that cause an infection in a Bartholin’s abscess are simply an overgrowth of the natural vaginal organisms. However, occasionally an infection called Gonorrhoea is found, which is transmitted through sex. All sexually active women who have had a Bartholin’s abscess are encouraged to have a sexual health screen to check for sexually transmitted infections once the abscess has resolved at a sexual health clinic. These clinics are also able to contact sexual partners anonymously to advise treatment if your swabs confirm a sexually transmitted infection.
Are there any other treatment options?
An operation called marsupialisation is the alternative treatment. This will involve a general anaesthetic. The procedure again involves making a cut into the cyst/abscess and dissolvable stitches are used to hold the abscess/cyst cavity open after the fluid/pus has drained out. The stitches dissolve over 4 weeks and the aim is to help the abscess/ cyst heal in such a way that reduces the chance of it forming again. Marsupialisation is needed for complex or unusual abscesses, when a word catheter has failed or if you just do not want a word catheter.
The disadvantages of this procedure include the risks of a general anaesthetic. You will also need someone to collect you after surgery and stay with you for 24 hours; this is because a general anaesthesia can affect your memory, concentration and reflexes for up to 1–2 days. Thirdly, while waiting for your emergency operation, more urgent cases may need to take priority. During this time, the abscess may spontaneously split open and drain; this is not predictable. Marsupialisation is usually cancelled when this happens because it is less successful.
Patient Advice & Liaison Service (PALS)
If you have concerns or wish to give feedback about services, your care or treatment, you can contact the PALS office in the main atrium or you can complete a feedback form on our website www.chelwest.nhs.uk/pals. We value your opinion and invite you to provide us with feedback.
WM: 020 8321 6261; chelwest.wmpals@nhs.net
C&W: 020 3315 6727; chelwest.cwpals@nhs.net
Useful contacts
The Elizabeth Suite, Chelsea and Westminster Hospital (Early Pregnancy and Acute Gynaecology Unit)
West Middlesex University Hospital (Early Pregnancy Unit)
Tel: 020 8321 (6070) or (6506), 07920 020800

