Bunion Management
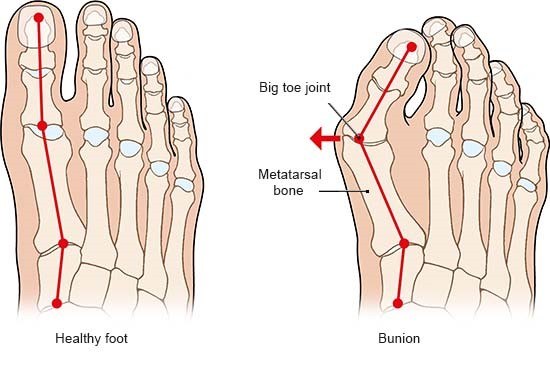
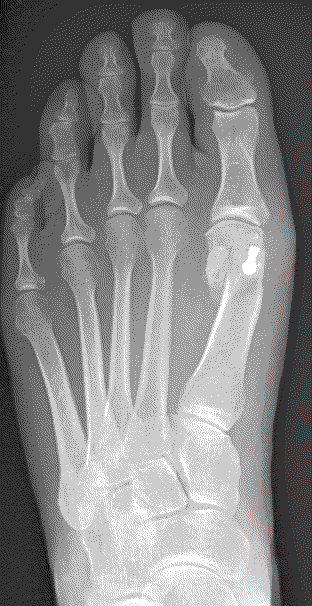
The severity of the condition is assessed by an X-ray. There is no direct correlation between the size of the deformity and the degree of symptoms experienced.
Treatment options
Conservative care
Conservative care is aimed at managing the symptoms only.
- Wide fitting shoes
- Insoles
- Night splints (children)
- Painkillers and anti-inflammatories
Surgical Management
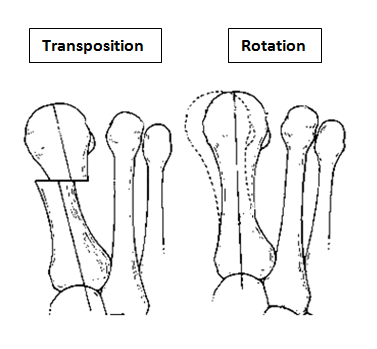
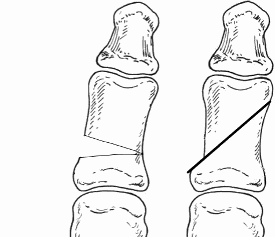
The aim of the surgery is to realign the first metatarsal almost parallel to the second metatarsal. This will move the big toe back into a straight position. This is achieved by cutting the bone. Sometimes re-balancing the soft tissue around the joint or taking a small wedge of bone out of the big toe is also required (Akin). The outcome of your operation will be dependent on the quality of your joint, the degree of arthritis present. There are numerous operations to correct bunions, but essentially, they fall into two categories: transposition and rotational procedures. Transposition osteotomies include the ‘Scarf’ and the ‘capital’. Rotational procedures include the ‘Lapidus’.
A transposition osteotomy such as a Scarf or capital osteotomy is where the bone is cut and moved across. The amount of correction available is restricted by the width of the bone. It is ideally suited to moderate deformities. In severe cases a rotational procedure such as a ‘Lapidus’ is preferred. Here a greater degree of correction is available. This operation also takes longer to heal and to settle down. Either procedure may be combined with an ‘Akin’ to help move the big toe to a straight position.
You will be advised on the appropriate procedure to correct your deformity. Ultimately, it is your decision as to whether you proceed with surgery or continue with conservative care.
Alternative procedures
In the Department of Podiatric Surgery, the common procedures carried out are the three described in this information booklet (capital, Scarf and Lapidus).
There are other options available. One type of procedure which has gained popularity in the media is ‘Minimally Invasive Surgery’ (MIS).This involves one or more small incisions to cut the bone under X-ray guidance, with the objective to reduce surgical and recovery times. However, a number of evidence based reviews show that MIS has high rates of complications including recurrence of the bunion (up to 60%), poor alignment (up to 61%) and stiffness in the big toe joint.
Possible outcomes
Depending on the quality of your big toe joint i.e. the presence and degree of ‘wear and tear’ arthritis, the risk of joint stiffness and/or pain in the big toe joint following bunion surgery will be increased. If the arthritis is severe, you may be offered an alternative procedure such as a big toe joint fusion. Everyone having bunion surgery should expect some reduction in range of motion at their big toe joint. It is also possible that pain may be transferred to another part of the foot. This may be temporary, as you walk slightly differently during recovery. In some cases this is permanent, or requires further surgery.
Day surgery
You will be admitted to the hospital and discharged on the same day as your operation. On your arrival, you will be shown to the ward and asked to change into a gown. The team will confirm your consent, answer any remaining questions, and mark the surgical site(s).
Anaesthesia
You have the option of having a local (staying awake) or general anaesthetic (going to sleep). In either case the operation is normally carried out as a day case.
General Anaesthesia
On the day of your surgery, prior to having a general anaesthetic, you would be reviewed by the anaesthetic team to ensure that you are fit and well. You will be given all the relevant information on general anaesthesia and the opportunity to ask questions.
Whilst you are asleep we will administer local anaesthetic around your ankle to help reduce post-operative pain. When you wake up in the recovery ward, you will find your foot is numb and this may last between 12 and 36 hours.
Local Anaesthesia
A member of the team will anaesthetise your leg via an injection in the back of your knee (Popliteal block). This will be carried out with adequate time given to allow the local anaesthetic to take effect.
As the anatomy behind the knee varies a little from person to person we use a nerve stimulator to locate the nerves. This sends a small electric current down the needle which stimulates the nerve. This means that the muscles controlled by the nerve begin to contract and relax causing the foot to ‘flick’. This helps us deliver the anaesthetic with precision.
Local anaesthetic at the level of the knee not only blocks sensation but also movement of your foot. This can last between 12 and 36 hrs.
The operation
The standard incision is on the inside of the foot over the bunion deformity. The incision is normally between 4 and 10 cm in length, depending on the type of procedure you are having. Dissolving sutures are used to close the skin. The operation normally takes about 40 minutes.
Capital osteotomy
This is an osteotomy in the metatarsal head (transposition), the metatarsal head is moved to correct the deformity and fixated with a single screw. It is indicated for mild to moderate deformities. The choice to carry out a Scarf or a capital osteotomy will be made by your consultant.

Scarf osteotomy
This is a transposition osteotomy. It is normally indicated for mild to moderate deformities. The new position of the first metatarsal is maintained with two screws which enables stability.


Possible risks following capital and scarf osteotomies
Although these are stable osteotomies, however, a fracture is a possibility particularly in patients who are very active in the initial stages of the recovery or with weaker bone. In some the alignment is lost and requires another surgery to fix. Joint stiffness and pain in cases where there is arthritis present prior to surgery. Once the bone has fully healed, the screw(s) are no longer required. However, we only remove fixation if it causes irritation.
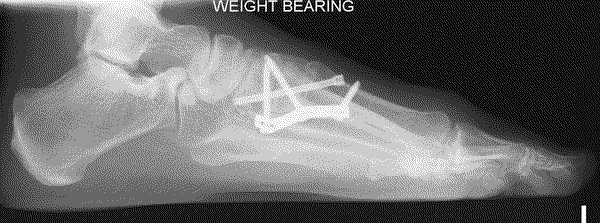
Lapidus (metatarsal cuneiform fusion)
This involves a fusion of the first metatarsal cuneiform joint, allowing the first metatarsal to be rotated back into a straight position. It is normally reserved for severe deformities. Once the corrected position has been obtained it is usually maintained with a plate and screws.
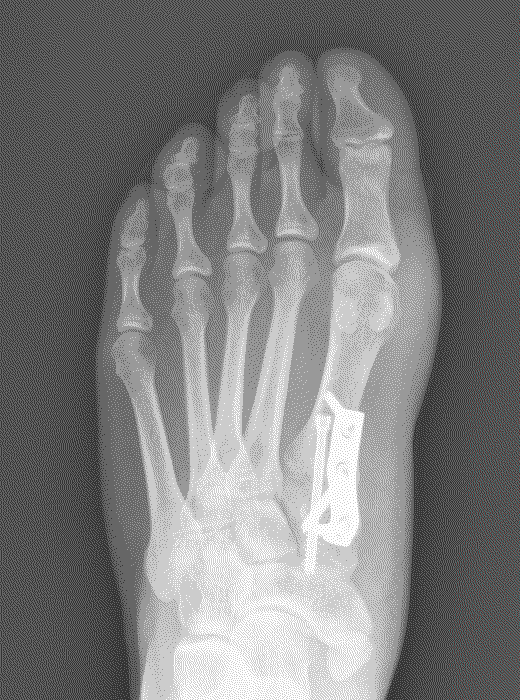
Possible risks with a Lapidus
Due to the corrective power of this procedure, there is a risk of overcorrection of the bunion, which may result in poor alignment with associated pain and arthritis in the big toe joint. A failure of the two bones to unite (non-union) can result in poor alignment and pain. In our department the audited risk of a non-union is 2%, which is lower than the average reported rate of 3.8%. A non-union may require revision surgery.
Outcome
An audit using a 100 point clinical rating system was used to assess pain, function and alignment, a score of 100 being perfect. The average score before surgery was 47.33.
Following the surgery the average outcome was 91.08 within our department.
Additional procedures
The ‘Akin’ Osteotomy is combined with a Scarf, capital or Lapidus to improve alignment of the big toe. A small wedge of bone is removed and fixed with a wire. This does not change the post-operative regime.
Discharge
Before you leave the hospital, you will be given an Aircast Walker following the Scarf and Lapidus procedures or a post-operative sandal in the case of a capital osteotomy. You will be shown how to partially weight bear on the foot using crutches. Post-operative painkillers will be dispensed by the nurses along with your next appointment.
You should arrange to go home by car or taxi with an escort. You should have someone with you for the first 24 hours in case you feel unwell.

Recovery
You must rest with the leg elevated for the first 48 hours (essential walking only). It is important that you do not interfere with the dressings and keep them dry. You can buy a purpose made waterproof cover to keep the leg dry, from your chemist (Limbo M100 above the knee).

Full recovery takes between seven to twelve months.
Possible complications
Approximately 700 patients undergo foot surgery annually within the Department of Podiatric Surgery at West Middlesex University Hospital. Most patients have an uneventful recovery. Outlined below are the common surgical problems or those rare complications with serious outcomes. In cases where we don’t have accurate audit we have used published results from the podiatric literature. These are accompanied by an asterisk *
- Prolonged swelling taking more than 6 months to resolve occurs 1 in every 500 operations*
- Haematoma - a painful accumulation of blood within the operation site.
- Thick and or sensitive scar.
- Infection of soft tissue.The incidence is 1 in every 83 operations*
- Delayed healing of soft tissue.
- Circulatory impairment with tissue loss occurred in 3 out of 9000 patients over a 10 year period.
- Venous thromboembolism (VTE) (a blood clot within the veins) may affect the legs or the lungs and is potentially a life threatening condition. Within the published literature, the overall incidence of VTE is thought to be 0.9% in foot and ankle surgery.
- Chronic pain syndrome: this is where the nervous system dealing with pain over reacts in a prolonged manner often to a minor incident.This normally requires management by specialist in this condition and doesn’t always resolve. This is a rare complication with no audit data available.
Specific complications following bunion surgery published in the literature
- Infection (2.6%*)
- Non-union of bone following the Lapidus (3.8%*)
- Delayed union (slow healing)
- Fracture
- Joint stiffness and pain
- Reoccurrence of symptoms or deformity (4.9%*)
- Fixation irritation (3.8%*)
- Transfer pain (6.3%*)
The risk of having a complication can be minimised when the patient and all those concerned with the operation and aftercare work together. This starts with the pre-operative screening and continues through to the rehabilitation exercises.
Pre-operative screening of your health allows us to determine whether you are fit for surgery. It is important that you disclose your full medical history. If there is a query regarding your health, then further investigations or the advice of other surgical and medical specialties will be sought. The surgeon and the theatre team will ensure that the operation is performed effectively and with the minimum of trauma.
You can improve the healing process and reduce the risks of complications by:
- Adhering to the post-operative instructions which include resting and elevating the operated leg. Keeping the wound clean and dry until advised otherwise is essential. Please ask the nurse or Podiatric surgeon if you are not sure what to do.
- Having a healthy diet is important. This provides the nutrition required for healing.
- Smoking is associated with a 20% increased risk of delayed or non-healing of bones.
- Alcohol can interact with the drugs that we will prescribe and in excess can impair wound healing.
- Post-operative mobilisation will be advised. This helps improve the flexibility, strength and stability of your foot.
Podiatric surgeons evaluate, diagnose, prevent and treat diseases, disorders and conditions affecting the foot and all associated structures. This is carried out in keeping with the individual’s education, training and experience, in accordance with the ethics of the profession and applicable law.
Podiatric surgeons are not medical doctors.
Podiatric Surgical Training
- 3 year: Degree in Podiatry (BSc)
- 2 year: Masters in the theory of podiatric surgery (MSc)
- 2 year: Surgical training programme (Podiatric Surgical Trainee)
Final fellowship examinations (Podiatric Surgeon) - 3 year: Specialist training (Podiatric Registrar)
- Accreditation with the Directorate of Podiatric Surgery
- Consultant Podiatric Surgeon

