Reconstruction after Mohs surgery: Understanding the surgical options
Brief introduction to Mohs micrographic surgery
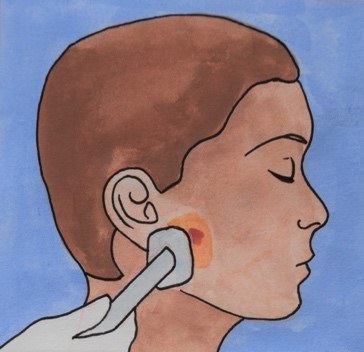
Mohs micrographic surgery is a surgical method used to remove some types of skin cancer most commonly basal cell carcinomas and squamous cell carcinomas. The procedure aims to preserve normal tissue and minimise chances that a reconstruction covers over a cancer.
The visible tumour is cut out, then thin layers of tissue around and beneath the wound are removed and analysed under a microscope to check that these margins are cancer free. If the surrounding tissue is not tumour free, a further layer is removed and analysed, this process is repeated until the margins are clear and the tumour has been completely removed. Further details on Mohs surgery can be found in the ‘Mohs micrographic surgery patient leaflet’.
The main advantage of Mohs surgery is that it guarantees full tumour removal and spares the healthiest tissue. This keeps more reconstructive options open, which can be particularly important in areas of cosmetic concern such as the face, or where spare local tissue is not available.
Reconstructive surgery aims to optimise the appearance of your scar. The risks of reconstructive surgery are similar to any other minor surgery, and will be discussed during your consultation.
Mohs Reconstruction
After the skin cancer is removed a wound is often left behind. A patient who has undergone Mohs micrographic surgery for a skin lesion may require reconstruction of the area. The reconstruction method used can vary depending on the size of the wound, its location and patient preference.
When Mohs surgery is performed on the nose, eyelid or ear, reconstruction is often recommended. Patients heal faster and have a better long term outcome with a reconstruction. Post-Mohs skin cancer reconstructive surgery aims to restore both the look and function of the skin after surgery.
Who performs the surgery?
Depending on the site, size of the wound and the method needed to close it, the reconstruction can be performed by the dermatology, plastic surgery or oculoplastic (if the wound is near the eye) team. In a teaching hospital this may be carried out by a trainee surgeon, with or without direct supervision from a Consultant.
Anaesthetic
There are three anaesthetic options for Mohs reconstructive surgery: local or general anaesthetic and local anaesthetic with sedation. The type you have will depend on factors such as the type of reconstruction, length of procedure and patient preferences.
Local Anaesthetic
Smaller reconstructions can be carried out under local anaesthetic, for example when the wound can be closed directly or with a small skin graft. Larger and more involved reconstructions and skin flaps are more commonly performed under general anaesthetic.
General Anaesthetic

With most surgeries performed under general anaesthetic you can go home later the same day or the following morning.
You are likely to feel drowsy after the anaesthetic, so you will not be able to drive home. You will also need a friend or relative to pick you up and stay with you until you have recovered from the effects of the anaesthetic.
Sedation
The aim of sedation is to reduce patient anxiety and discomfort during the procedure, the medications used will make you feel relaxed and sleepy. These medications are usually given through a vein (intravenously or IV), however they can also be given through a mask or orally, through the mouth. Unlike general anaesthesia, with sedation you remain semi-conscious and continue to breathe for yourself. Often you will not remember the procedure.
How long does it take?
The length of time the reconstruction takes depends on the size of the wound, location, complexity of the operation and what kind of anaesthetic you have. In general the surgery takes 1-2 hours. However, you should be prepared to set aside an entire day for the procedure and recovery time. You should be able to go home the same day of the operation.
Cleaning and Preparation
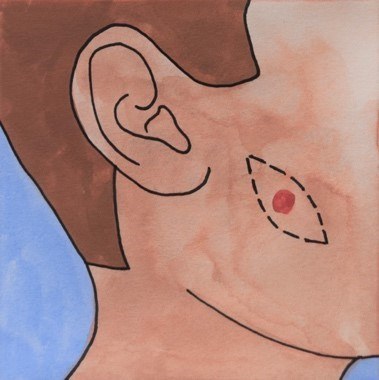
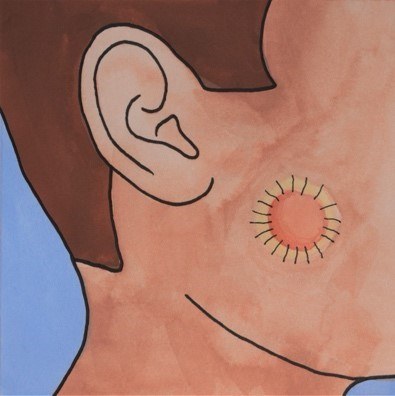
If the wound edges can be closed, they will be stitched together directly. This means the wound is closed edge-to-edge with a line of stitches. Often, the wound left after Mohs tumour removal is round or oval shaped.
To prevent the ends of the wound bulging when stitched together, the surgeon will make the wound an ellipse, adding two triangles to the opposite ends of the wound. This means the scar will be slightly longer, but it will lie flatter and have a better appearance.
Where possible, the surgeon will close the wound so that the scar lies in a natural skin crease. This technique is commonly used by the dermatology team and may not need input from the plastic surgery team.
Skin Grafts
This method may be used when a direct closure or local flap is not possible. The surgeon will take a piece of skin from another area of the body to cover the wound. After a few days the grafted skin connects to the skin around and beneath it and finds its own blood supply. As the grafted wound heals, it will slowly start to feel and look like normal skin again; this process may take months to complete. There are two types of skin graft, split thickness and full thickness.
Split Thickness Skin Grafts
This is a thin layer of shaved skin which allows healing beneath it. The graft skin is placed over and stitched to the Mohs wound.
Where can the graft be taken from?
The area where the graft has been taken is called the ‘donor site’. The upper outer thigh is a common donor site, although other areas can be used, including the outer thigh, calf, scalp and arms.
Is a split thickness skin graft painful?
The donor site can be sore, like a raw graze, and some people report a burning sensation. The donor site will be dressed following the surgery. The soreness often lessens after 2-3 days, as the wound begins to heal. The donor site will usually heal after 2-3 weeks, and the dressing should fall off by itself.
How is a split thickness skin graft attached?
A split thickness skin graft consists of a very thin sheet of skin which is draped over the wound and attached. For some grafts, a special skin glue can be used to hold the skin graft in place. Stitches may also be used (dissolving, non-dissolving or a combination of the two). In addition, stitches can be used to attach a dressing onto the graft, preventing it from being moved or damaged during healing.

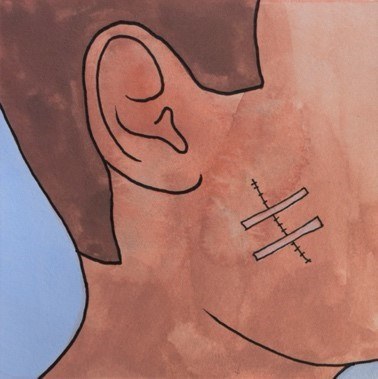
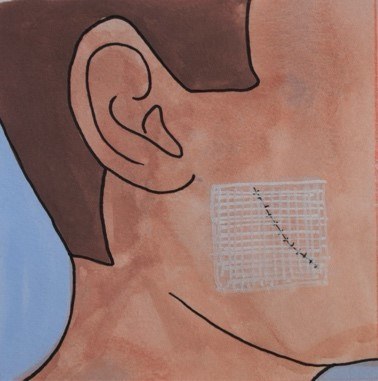
Full Thickness Skin Grafts
This graft uses the entire thickness of the skin, not just the top layer as in a split thickness skin graft. It involves cutting out a piece of skin and stitching the donor site wound up. The graft is then placed in the wound from the Mohs surgery and sutured to the surrounding skin to hold it in place.

Why is a full thickness skin graft used?
Full thickness grafts can maintain more of the normal features of skin when they are transplanted, such as thickness, texture and hair growth. They might be a good choice for highly visible parts of the body such as the face. However, they require a greater blood supply so need good conditions in order to survive.
Where is a full thickness skin graft taken from?
Full thickness skin grafts are commonly taken from spare skin around the neck and collar bone, around the ear, upper arm and groin.
Is a full thickness skin graft painful?
The donor site can feel sore but should settle down after 2-3 days. A full thickness skin graft donor site typically takes 3-4 weeks to heal. It is recommended that patients avoid strenuous activity for at least 2 weeks after surgery.
How is a full thickness graft attached?
A full thickness graft can be held in place by stitches (dissolving, non-dissolving or a combination of the two). Stitches may also be used to keep a dressing in place. However, unlike a split skin graft, a full thickness graft will be a similar shape to the wound left by the Mohs surgery.
How does a full thickness skin graft work?
During the first few days after the operation, new blood vessels form from the wound to the graft, keeping it alive. This process usually takes 4-5 days. Over the following weeks and months the grafted skin becomes stronger and will look more and more like normal skin. Scar tissue may also form in the area which may cause the graft skin to shrink and appear bumpy.
Local Flaps
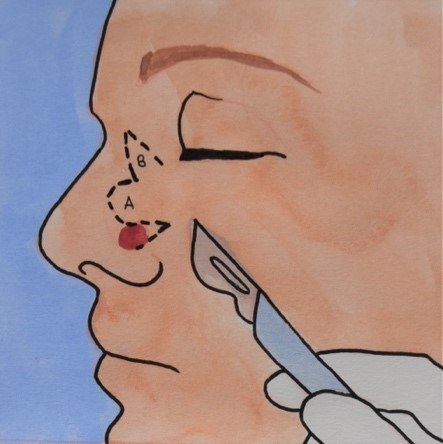

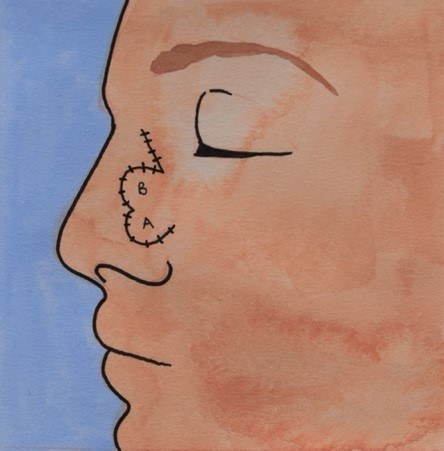
A local skin flap involves lifting and moving healthy tissue that is next to, or nearby the wound, to cover the area of missing skin. The skin flap remains attached to the area it came from, so it still has its original blood flow, which keeps the flap alive.
Where possible, flaps are chosen from adjacent sites because the skin is a good match in both colour and thickness.
A flap can be a number of different sizes and shapes depending on the laxity (looseness) of the local skin as well as the size and location of the wound.
Stiches and dressing
Stiches
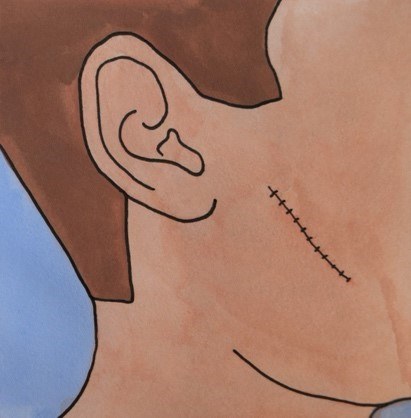
The type of stitches used will vary depending on wound size, location and surgeon preference. Usually dissolving stitches are used deep within the wound to hold it together. These stitches dissolve after 1-2 months and do not need to be removed.
Dissolving or non-dissolving stitches can be used to bring the skin together, these are the stitches you will see on the outside of the wound. Non-dissolving stitches will usually be taken out 5-10 days after reconstruction. This will take place at your GP or at the follow up clinic appointment. Dissolving stitches on the surface dissolve in 2-3 weeks.
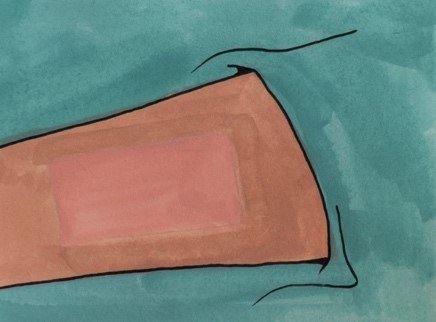
Dressing

The reconstruction site will be dressed after the procedure in the operating theatre. If a graft is used, the donor site will also be dressed at this time. The dressing protects the site. The types of dressing used varies based on the options available at the hospital and the surgeon's preference. Gauze, steri-strips (which look like pieces of tape), non-stick dressings and foam (to cushion the wound) can all be used. Sometimes only an ointment is required.
Usually it is advisable to keep the wound dry until seen in a dressings clinic. The surgeon will also discuss when the dressing will need to be changed, if you can change it yourself, or if you need a nurse to change it. This can be carried out in a GP or clinic setting.
What can the complications be?
A small amount of bleeding and discharge of fluid from the surgical site into the dressing is common. More serious bleeding is rare. Pain or tenderness, either from the wound or from a donor site (if a skin graft was used) can also occur.
As with any wound, there is a small risk of infection. This can be reduced by good blood sugar control if you are diabetic and stopping smoking. Antibiotics are sometimes (but not always) given before, during or after surgery to reduce infection risk.
With all surgeries you will have a scar that fades over time. Problems with wound healing may cause the scar to open up and damage underlying structures, such as nerves and blood vessels, which may cause numbness. Factors such as being underweight or malnourished may contribute to poor scar formation.
Rarely, there may be bleeding under the skin, forming a collection of blood called a haematoma. This may cause the graft or skin flap used in the reconstruction to work less successfully than planned.
Sometimes the reconstructive surgery has to pull or move tissues to cover the hole and this may distort facial features such as the eyelids, nose and mouth. It is normal to have swelling around the wound site for several months, especially if the area around the eye is involved.
The aim of this reconstructive process is to improve the look of the final scar, however the end result cannot be predicted. The area will have a different appearance compared to the skin before the cancer was removed and there is a possibility that you may not be happy with the final result.
Scar Formation and Management
A scar is expected with any surgery, but our aim is to minimise its appearance.
From 0-14 days, the scar may appear red, swollen and might still be sore. Scabs may form in the later half of this stage.
Between 2-3 months, all scabs will settle and the scar lines will look pink and raised.
Between 3-12 months the scar should fade and flatten.
Once the scar has healed (2 weeks), moisturising the scar with lubricants such as oils, or a hypo-allergenic (non-perfumed) moisturiser, e.g. aqueous cream, is recommended. After 3-4 weeks moisturiser can be massaged into the wound for 5 minutes, twice a day for up to 4 months.
In addition, silicon gel or dressings can be used to hydrate the scar.
Sun protection for the first year after surgery is very important. SPF50 or a covering such as a hat is highly recommended to avoid burning the scar.
FAQs
Q: Will Mohs reconstruction leave a scar?
A: Yes. Every surgery leaves a scar. You can improve its appearance by following the steps in the 'Scar Formation and Management' section of this leaflet.
Q: How long will the surgery take?
A: Usually the surgery takes 1-2 hours. You should be able to go home the same day as the procedure.
Q: Will I be awake for the surgery?
A: This depends on the type of anaesthetic used: local anaesthetic (where you are awake) and general anaesthetic (where you are asleep). Anaesthetic is used to reduce pain during and after the surgery. More complex reconstruction methods such as local flaps will need a general anaesthetic.
Q: Is the surgery painful?
A: You can expect some discomfort after the procedure. The surgeon will use local anaesthetic to numb the area being operated on to reduce pain. Pain can usually be managed with over-the-counter pain medications such as paracetamol and Ibuprofen.
Q: Should I take my usual medications before the surgery?
A: Most procedures are done under local anaesthetic so eating, drinking and medication on the morning of the surgery is acceptable. However, blood thinners such as Warfarin and Apixaban may need to be stopped. This should be discussed with your Doctor.
Q: I have a pacemaker. Will this be a problem?
A: Your Doctor should be aware that you have a pacemaker as the surgical equipment can interfere with its signal. This might require a pacemaker technician to be present on the day to service the device.
Q: What should I do if I have concerns or experience complications such as infection, excessive bleeding or unmanageable pain after my operation?
A: You can contact:
(Mon-Fri) The Plastic surgery Clinical Nurse Specialist: 07385384435/ 07824502944
(Mon-Fri) The Plastics dressing clinic: 02033152788, email - PDC@chelwest.nhs.uk
(Weekend/Emergency): Attend A&E


