Troubleshooting continuous subcutaneous insulin infusion (CSII)
Factors for success on CSII
People do better on an insulin pump if they:
- Monitor their glucose regularly (at least 4 times /day)
- Use of the bolus calculator to calculate insulin doses
- Use bolus doses for all carbohydrate intake
- Change the infusion set regularly and every 2-3 days, ideally early in the day
- Use of advanced features: temporary basal rates & dual wave boluses
- Attend their clinic appointments regularly
- Downloads and review their data regularly
Pump failure
If your insulin pump stops working for any reason it is essential that you have a backup plan. As only quick acting insulin is in your pump, without this, your levels can start to rise quickly, and ketones can start to form within 4-5 hours.
- Administer long acting insulin (Glargine or Detemir) using a pen or syringe. Your total daily amount of basal insulin should be administered. If you do not have long acting insulin with you then check glucose levels every 3 hours and take a dose of rapid acting insulin.
- Continue with your usual carbohydrate ratio and correction factor using a pen or syringe.
- Contact the insulin pump company via their helpline about a replacement pump (this may take 1-2 days)
- Once you have your replacement pump you will need to set this up with your rates. These can be found on your last clinic letter, so please keep a record. The information may also be found if you have done a recent upload.
Please make sure you carry your back up pens with you & check expiry dates
Management of unexplained raised glucose levels
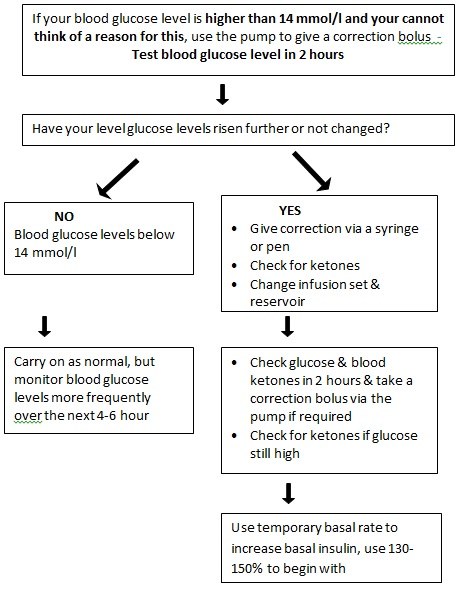
Follow sick day rules if ketones are positive
Do not got to sleep:
- with unexplained hyperglycaemia which has not resolved , or
- within 2 hours of a new set change
Identifying causes to raised glucose levels:
- Are you having difficulties with the insulin pump itself?
- Is there an air bubble in the infusion set?
- Is the cannula inserted correctly or has it slipped out due to perspiration?
- Is there a blockage or a leakage?
- Is your pump in suspend mode?
- Are the infusion set and adapter connected properly?
- Is the infusion set compatible with the reservoir?
- Did you prime the infusion set when you changed the set?
- Has the infusion set been placed in an area of hard/lumpy skin?
- Has the insulin itself been exposed to extreme temperatures?
- Is the reservoir empty?
- Is there any blood in the infusion set?
- Has the needle/cannula been in for more than 72 hours?
- Has the infusion set kinked?
- Has the battery run down?
- Has the insulin expired?
Carry out a self-test to check that the pump is functioning properly.
If you are concerned that the pump may not be working, please ring the manufacturer’s pump support line immediately.
Sick day rules
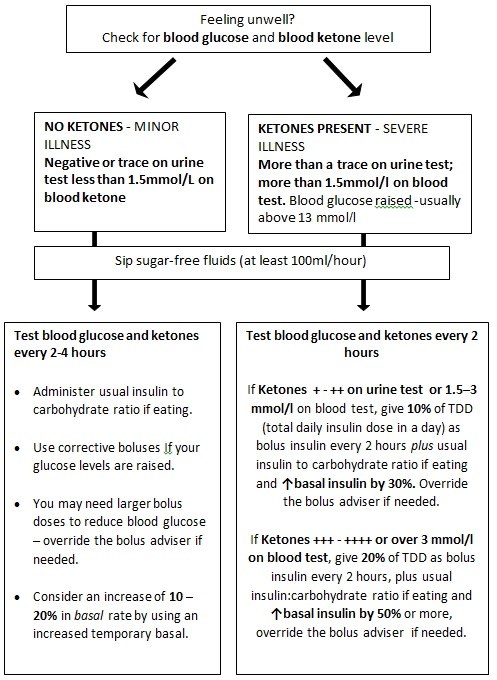
Drink plenty of sugar-free fluids (a minimum of 100 mls per hour).
If not hungry, take small amounts of carbohydrate-containing fluid often (e.g. fruit juice, ice cream, Lucozade etc.)
Contact Diabetes team (020 3315 8132) during working hours if unsure.
If you continue to vomit, are unable to keep fluids down, or unable to control your blood glucose or ketones you must go to the hospital as an emergency.
You must never suspend/stop your pump.
Hypoglycaemia
Causes of hypoglycaemia:
- Overestimating the carbohydrate content of your meal/snack/drink.
- An increase in physical activity without changes to your basal rates and/or carbohydrate intake. Remember, even light activities e.g. gardening, shopping etc. may require a temporary basal rate.
- Consuming significant amounts of alcohol without reducing insulin delivery temporarily.
- Administering a standard/normal wave insulin bolus for a high fat, high protein and or low glycaemic index meal.
- Giving too much of a correction bolus for a high blood glucose level or correcting a rebound high following a previous hypo.
- Errors handling the pump e.g. two boluses for the same meal or programming an incorrect bolus dose.
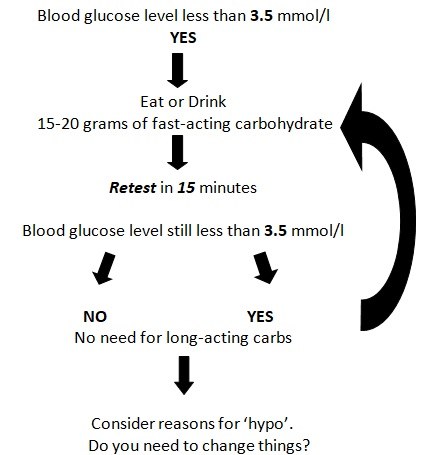
The important thing to remember is to recognise when you are low & treat hypos as quickly and as effectively as possible.
Hypo warnings may change if hypos are frequent, they can become more subtle.
Use the 15:15 rules: Aim for 15-20 g quick acting carbohydrate repeated every 15 minutes until blood glucose levels return to base line. Complex carbohydrates do not need to be taken to maintain this level due to the slow release of the basal insulin on a pump during the day.
Examples of 15g of Quick Acting Carbohydrate:
- 5 glucose tablets: Dextrose, Lucozade tablets or
- 3-4 Glucotabs or
- 140ml Coca Cola (approx. ½ normal can)
- 170ml Lucozade (Not Lucozade Sport) or
- 140ml of fruit juice
Please check individual carbohydrate content on item packaging as there may be discrepancies.
Suspending the pump will NOT prevent/treat hypoglycaemia because the action is not quick enough.
If a pattern of low blood sugar is detected and thought to be related to the basal rate, the basal rate should be reduced by ± 0.05 – 0.1 units/hour or 10-15% about 60 – 120 minutes before that time period. However, in the case of a night time hypo that cannot be attributed to alcohol, increased activity the previous day or an error in meal estimation, please immediately reduce the basal rate the following evening.
Steps to prevent hypoglycaemia
- Test blood glucose regularly and always before driving and going to bed.
- Check if your insulin to carbohydrate ratio for meals is correct.
- Do not skip meals for which you have taken insulin.
- When exercising, test blood glucose before, during, and after activity and be aware that prolonged exercise may also lead to low blood glucose levels many hours later.
- Be aware of alcohol consumption and carry out an extra test.
- Do not start a car journey driving with blood glucose below 5.0 mmol/l. If it is a long car journey, then test blood sugars every 2 hours.
- Excessive heat (sauna, bath, sun and so on) increases the rate insulin is absorbed and may cause hypos
In relation to the pump:
- Check the pump’s alarms to see if an error has been identified.
- Maximum bolus and basal rates can be re-set to prevent you from administering too much insulin.
- Always treat a hypo before adjusting the pump setting.
Share this information on hypo treatment with close family and friends so that they can assist you, if necessary, to treat a hypo safely. Show a close friend or family member how to administer Glucagon and Glucogel and where it might be kept.
Remember to carry quick acting carbohydrate with you at all times for treating hypoglycaemia.
Hypo treatment flow chart. Always treat hypos immediately
Troubleshooting on an insulin pump
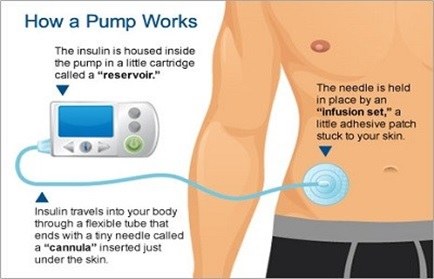
How insulin pumps work. Image courtesy of Liberty Medical

