Bowel Endometriosis
What is endometriosis?
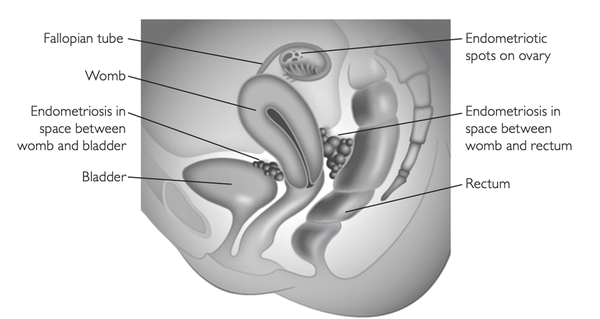
Endometriosis is a condition where tissue similar to the inner lining of the womb (endometrium) is found elsewhere, usually in the pelvis around the womb, ovaries and fallopian tubes. It is a very common condition, affecting around 1 in 10 women. You are more likely to develop endometriosis if your mother or sister has had it. It can be a long-term condition that can have a significant impact on your general physical health, emotional wellbeing and daily routine.
Less commonly, endometriosis can affect the bowel in the abdomen and pelvis. The endometriosis can be superficial (on the surface of the bowel) or deep and invade into the bowel wall and surrounding tissue. The most common site for deep endometriosis is in the space between the rectum and vagina.
Figure 1: Endometriosis (RCOG)
What are the symptoms of bowel endometriosis?
Endometriosis can affect patients in a variety of ways. In some there are no symptoms, others their fertility is affected. With bowel endometriosis the usual symptoms are pain on opening the bowels (dyschezia) and deep pelvic pain with sex (dyspareunia). Although bowel endometriosis can be associated with bleeding from the rectum during a period this is perhaps more commonly caused by haemorrhoids (piles) and other bowel conditions.
Please inform your team if you have this symptom and the team will discuss with you if further tests are needed. Symptoms may vary with the menstrual cycle and are typically worse in the days before a period and during menstruation.
Will I be examined and what tests may I be offered?
Your specialist nurse or doctor will ask you about your symptoms. They may also ask you if they can perform an internal examination of the vagina to assess endometriosis between the vagina and the rectum. A digital rectal examination may also be necessary.
They may arrange further appointments for an ultrasound scan (a transvaginal scan where the probe is gently inserted into the vagina) or an MRI (you will lie inside a large tube that uses magnetic fields to give detailed images of the pelvis, https://www.nhs.uk/conditions/mri-scan/. When endometriosis is superficial these scans may be normal. The imaging offered will depend on the symptoms you have and whether examination suggests deep disease.
As endometriosis can affect the bowel, bladder and ovaries in many ways your treatment schedule will often be discussed by a number of specialists in a multidisciplinary meeting which is attended by consultant gynaecological surgeons, consultant bowel surgeons, consultant radiologists and the specialist endometriosis nurse.
Following this meeting a sigmoidoscopy or colonoscopy may be suggested. This is a day case procedure carried out by the bowel surgeons where a small camera is passed up through the back passage (anus) to examine the inside of the bowel. These tests can provide further information about how much of the bowel wall is involved, or whether there are any other causes for your symptoms.
The team will use this information to discuss with you what type of surgery may be required and what the risks may be. However, a full assessment of endometriosis will only be possible at the time of surgery.
What are my options for treatment?
Endometriosis is a chronic condition and, in that sense, there is no cure. It can be difficult to treat but the symptoms can be reduced with the correct management. Different treatments will be more appropriate for different women, and the right treatment for you may change over time.
- Pain relieving medication: these can range from paracetamol and ibuprofen that you buy over the counter to stronger painkillers such as codeine that may be prescribed for you. In more severe situations you may be referred to a specialist pain management team.
- Hormone treatments: these treatments reduce or stop ovulation (the release of an egg from the ovary) and therefore allow the endometriosis to shrink by decreasing hormonal stimulation. They will not cause the endometriosis to disappear and symptoms will return if treatment is stopped.
Some are contraceptive and will stop you from getting pregnant:
- The combined oral contraceptive (COC) pill or patch given continuously without the normal pill-free break; this usually stops ovulation and temporarily either stops your periods or makes your periods lighter and less painful.
- An intrauterine system (IUS/Mirena®), which helps to reduce the pain and makes periods lighter; some women using an IUS get no periods at all
- Progestogens in the form of injection, the mini pill or the contraceptive implant.
Some are not contraceptive, and you should use contraception if you do not wish to become pregnant.
- Progestogens in the form of tablets
- GnRHa (gonadotrophin-releasing hormone agonists), which are given as injections, implants or a nasal spray. They are very effective but can cause menopausal symptoms such as hot flushes, night sweats, vaginal dryness and effects on mood. They are also known to reduce bone density. To help reduce these side-effects and bone loss, you may be offered ‘add-back’ therapy in the form of hormone replacement therapy (HRT). For this reason they are not commonly used for longer than 6–9 months.
- Surgery: the aim of surgery is to cut out (excise) or destroy (ablate) as much of the endometriosis as possible. We aim to excise endometriosis but there will be a few cases where it is safer or more appropriate to ablate. Even if all the endometriosis is removed it will recur in some women. Surgery for bowel endometriosis is discussed further below.
- Complementary therapies: some women may find that therapies such as reflexology, acupuncture and herbal treatments reduce their pain or improve their quality of life. However there is a lack of scientific data to show that they are effective.
Does bowel endometriosis have to be treated? What are the risks of not having treatment?
Whether or not bowel endometriosis requires treatment depends on your particular case, your symptoms and how severe the endometriosis is. Your doctor is there to try and help you and explain the treatment choices. The final decision is yours.
Without having treatment, your symptoms are likely to continue and may get worse. Endometriosis gets worse in about half of women and this may mean that deep endometriosis extends further into the bowel becoming more difficult to treat. Research also suggests that endometriosis may get better as well as worse over time.
Surgery for Bowel endometriosis
Most surgery can be carried out laparoscopically – key-hole surgery with three to four small incisions in your abdomen. Most commonly there will be a 1-2cm incision in your umbilicus (belly button) and two to three smaller incisions lower down. The advantage of laparoscopic surgery is that you will recover quicker afterwards, it will be less painful and less scar tissue (adhesions) will form inside your abdomen.
In some cases it will be necessary to make a larger cut on your abdomen – a laparotomy or open surgery. This may be planned in advance or become necessary during the procedure. Your surgeon will discuss with you how likely this is to occur.
Your surgery will be performed by a gynaecologist who specialises in endometriosis surgery. In some cases there will also be a bowel surgeon present.
Depending on how deep the involvement of the bowel is there are three surgical options:
- Rectal shave: in many cases the nodule of endometriosis can be ‘shaved off’ the bowel without needing to open the inside of the bowel. The endometriosis is cut out using either laser or scissors. Occasionally this may result in a small amount of endometriosis being left on the bowel. Sometimes stitches will be placed in the bowel if the wall is very thin or there is a small hole in the bowel.
- Disc resection: for deeper nodules of endometriosis a disc of bowel wall can be removed and then the hole closed with either stitches or staples.
- Segmental resection: with some deep or large areas of endometriosis, particularly if they are causing narrowing of the bowel, it may be necessary to remove a segment of the bowel and then re-join the two ends of bowel (anastomosis).
With bowel surgery there is a possibility that a temporary colostomy will be needed. This is a procedure where a section of the bowel is attached to an artificial opening on the tummy wall. This opening is known as a stoma. A stoma bag stuck to the skin of your tummy collects faeces. If it is thought that you might need a stoma, your surgeon will arrange for you to talk to a specialist nurse. In most cases a stoma is not required. If a stoma is required it would be removed (reversed) within a few months.
In some cases the endometriosis may invade through the top of the vagina and it may be necessary to open the top of the vagina (near the cervix) to remove all the endometriosis. This hole will then be closed with stitches. If this is necessary you may have some vaginal bleeding after the operation, and should avoid sexual intercourse for 4 weeks to allow the vagina to heal.
If you are not planning to get pregnant soon after the surgery then it is recommended to use the combined oral contraceptive pill for at least 6 months because this will make pain less likely to return. Alternatively, a Mirena IUS (coil) can be inserted at the time of surgery, but this may not be as effective.
Before the surgery
You will meet with the surgeons to discuss the plan for surgery as well as the possible complications. You will usually be given at least three months of medical treatment before the surgery. This may be GnRH analogues or the contraceptive pill. The aim of this is to make the endometriosis less active so that the surgery is safer. You may be given bowel prep (Picolax or MoviPrep) which will help to empty the bowel. If the bowel is opened during the surgery there may be less chance of contaminating the abdomen. Instructions can be found at the end of this document.
What are the risks of having surgery?
The most serious risks of this complex surgery include leakage of the bowel contents from where the bowel endometriosis was removed (potentially life threatening), requiring a stoma (a temporary bag that drains the bowel contents). International data suggest injury to the bowel can occur in 5 in 100 cases, however in our experience at Chelsea & Westminster this is less common.
Up to 15 in 100 cases of bowel injury might not be diagnosed at the time of surgery. In some cases repair can be undertaken with the same small cuts in your skin (laparoscopically) and in other cases will require a large cut on your tummy (laparotomy).
A rectovaginal fistula can occur in 1–2 in 100 cases after a rectal shave but 10–15 in 100 cases of more complex bowel surgery and your surgeons will be able to tell you if they feel you are particularly at risk.
A fistula is an abnormal connection between the bowel and vagina and leads to gas or faeces leaking from the vagina. This is most likely if the vagina needs to be opened at the time of surgery. A fistula requires further surgery and a temporary stoma to repair.
Some women who require a segment of bowel to be removed may notice a change in their bowel habit, for example needing to open their bowels more frequently or needing to rush to the toilet. These symptoms may improve with time.
There is a risk of damage to the urinary system (bladder and ureters). The nerves that control the bladder can be damaged during the surgery and this may make it difficult to empty the bladder. Some women will need a catheter to drain the bladder for a period of time after the surgery.
Bleeding can occur at the time of surgery. It is unusual for this to be excessive but you should tell you surgeon if you have any objection to receiving a blood transfusion.
What to expect after the operation
You can expect to feel sore. You will have been given painkillers before you wake up and can have more in recovery until you are comfortable enough to go back to the ward. You can start drinking water soon after your operation and build up to eating. If you feel sick or do vomit after the operation, the nurses will administer anti-sickness medication into the drip in your arm to help reduce this.
You can expect to have a urinary catheter (a thin tube inserted into the urethra (the tube through which urine passes) to the bladder, allowing urine to flow through it and into a drainage bag) for the first night.
It is not uncommon for your bowels not to work for a few days after the operation. You may be prescribed a gentle laxative to help get your bowels moving. Drinking plenty of water also helps. You should avoid straining to go to the toilet.
The cuts in your skin will be closed by stitches that will dissolve over 7 to 14 days. The dressings should stay on for 72 hours after the surgery. You can shower with the dressings on and also once they have been removed. Gently pat the scar dry afterwards.
You may get a small amount of vaginal bleeding. This is because an instrument will have been placed through the vagina and into the womb during surgery to allow the surgeon to see all parts of the pelvis.
You can expect to have some pain in your lower abdomen. You may also feel some pain under the ribs and in your shoulder, this is because of the gas that is used to inflate your abdomen during the surgery. This will usually have resolved by 36-48 hours after the surgery.
When leaving hospital, you will usually be provided with painkillers for the pain you are experiencing. Sometimes painkillers that contain codeine or dihydrocodeine can make you sleepy, slightly sick and constipated. If you do need to take these medications, try to eat extra fruit and fibre to reduce the chances of becoming constipated.
You will be given compression stockings to wear to reduce the risk of blood clots forming in your legs. You will also be given heparin injections each day. You can reduce the risk of clots by:
-
Being as mobile as you can as early as you can after your operation
-
Doing exercises when you are resting, for example:
-
Pump each foot up and down briskly for 30 seconds by moving your ankle
-
Move each foot in a circular motion or 30 seconds
-
Bend and straighten your legs- one leg at a time, three times for each leg
Recovery time, both in hospital and at home, varies from one person to another. Don’t try and compare yourself to how others are recovering. After a rectal shave many women will feel ready to go home the day after the surgery. If removal of part of the bowel has been required it is usual to go home after 2-4 days, and after open bowel surgery (laparotomy) it may be longer.
By the time you go home you will be able to get up and about. You may be taking regular painkillers for the first few weeks. You can gradually return to normal daily activities. A gentle walk every day is beneficial; try and do a little bit more every day, but stop if you feel pain. If you drive you should check your insurance policy. In general you can go back to driving when you have stopped taking strong painkillers (which might make you drowsy), and can comfortably sit in the car seat and turn to look in the mirror and do an emergency stop.
You may feel much more tired than usual after your operation as your body is using a lot of energy to heal itself. You may need to take a nap during the day for the first few days. For many women this is the last symptom to improve.
How much time you will need to be off work depends on the type of work that you do and the extent of the surgery. You can expect to be off work for around two to four weeks after major bowel surgery. It may take a few months before you feel fully back to normal.
Bowel function may be altered following this type of surgery, particularly with a full resection (re-anastomosis). This does improve over time although women may need to watch their diet to see which foods aggravate or improve the situation. Some patients may benefit from the advice and support of a dietician. It is important to discuss any concerns with your consultant.
When to seek medical advice
Most women recover well after laparoscopy though complications can occur as with any operation. You should seek medical advice from the hospital or your GP if you are worried about your recovery especially if your symptoms are persistent and do not improve with time.
After going home, you should seek medical help if you have any of the following:
- A high temperature (more than 38°C)
- Not passed flatus (wind from your bottom or your stoma if you have one) for more than 48 hours and have abdominal pain
- Increasing abdominal pain/feeling faint/feeling increasingly unwell on the first postoperative night Risk: Bleeding internally
- Burning or stinging when you pass urine or pass urine frequently beyond 12-24 hours after your operation Risk: Urine infection
- Red painful skin around your scars, weeping of cut: Risk: Skin infection
- Abdominal pain that is getting worse, especially if you also have a temperature (fever), loss of appetite and feel sick or are vomiting. Risk: Bowel damage
- Have a painful, red, swollen hot leg or have difficulty bearing weight on one of your legs. Risk: deep vein thrombosis (clot on leg, DVT).
- If you have new symptoms of shortness of breath, chest pain or cough up blood some days after the operation. Risk: Pulmonary embolus (Clot on lungs, PE)
Contact details
- Endometriosis specialist nurse contact form
- Endometriosis specialist nurse: chelwest.endometriosis@nhs.net
- Annie Zunz Ward (for urgent post-operative advice): 020 3315 3905
Taking Picolax before your laparoscopy
You are required to take 2 sachets of Picolax (Bowels preparation) on the day before your surgery. Please follow these instructions carefully:
- You may eat a low residue diet up until 8am on the morning of the day before your surgery.
- Please take the first sachet of Picolax at 8am, the morning before your surgery—mix well into a glass of cold water (approx 150 ml) before drinking
- You are allowed clear fluids only after you start drinking the first sachet of Picolax, eg water, cordial, squash, weak tea and coffee with no milk, orange and apple juice without bits, jelly, and consommé (clear soup).
- Please take the second sachet of Picolax at 2pm on the day before your surgery.
- Remain on clear fluids only until 2am on the morning of your surgery. From 2–6am you must drink water only.
- You are to be nil by mouth from 6am on the morning of the surgery—this means no food, no water, no sweets or chewing gum.
- Please remember that up until 6am on the morning of your surgery, it is important to drink plenty of fluids in order to replace fluid lost from the body. In general you should try to drink a glass of water or other clear fluid (about 250 ml) every hour while the effects of the treatment persist.

