Biliopancreatic diversion
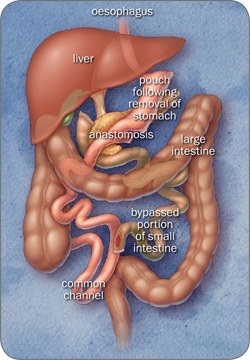
The first step creates a pouch. The surgeon uses metal staples that are similar to stitches and then cuts through the stomach. The new stomach pouch is about a quarter of the size of the original stomach. The remainder of the stomach is removed.
As with the bypass, the surgeon will then divide your small intestine and attach one end to the pouch. Food will now pass from your pouch into this section of small intestine.
The remainder of your small intestine, that previously was attached to the bottom of your stomach, now joins the other part of the small intestine close to the large intestine.
This means that your digestive juices join the intestine to mix with food right at the end of the small intestine. This way, absorption of food is greatly reduced.
The Duodenal Switch procedure is a variant of the Biliopancreatic Diversion. As with the original Biliopancreatic Diversion, this operation includes dividing the stomach but only the outer margin is removed, leaving a sleeve of stomach with the pylorus (valve between the stomach and intestine) and duodenum at its end.
The duodenum is divided so that pancreatic and bile drainage is bypassed. The near end of the alimentary limb is then attached to the beginning of the duodenum while the common limb is created in the same way as described before.
Patients can consume larger quantities than with other surgeries because the pouch is bigger and fat and sugars are not absorbed by the intestine.
As a result, patients may experience frequent loose bowel motions, especially in the first 6 months. Over time, the intestine will adapt to better absorb food and bowel movements will decrease to about 3–5 per day.
Expectations of weight loss
Following this operation people tend to lose weight quickly and lose 75–80% of their excess body weight after 5 years. However, the side effects that occur following this procedure mean it is generally not acceptable for most patients.
Advantages
- The amount of food you can eat is not restricted
- Weight loss starts from the time of surgery
- You can lose on average 75–80% of your excess weight
- You may be able to maintain your weight loss better than with other surgeries
- Resolution of diabetes in 95% of cases after 2 years
Disadvantages
- The surgery itself has more risks than the gastric band because it is a longer procedure and the stomach and intestines are cut
- Obstruction can occur where the new joins are created at the pouch and further down the intestine—this may require a procedure (endoscopic or surgical) to widen the area and allow food to travel through at the correct rate
- You will need to take many multivitamin and mineral supplements on a daily basis for life
- You will be at greater risk of suffering from nutritional deficiencies than the bypass, particularly iron, calcium, vitamin A and D and protein—close monitoring for protein malnutrition, anaemia, and bone disease is required after these operations
- Your hair may thin although this is temporary while losing weight at a rapid rate
- You may develop gallstones (this happens in 60% of cases) due to rapid weight loss—it may be necessary to undergo a further operation to remove your gallbladder, or it may be removed at the time of surgery
- Foul smelling flatulence and loose stools may be experienced especially if dietary changes have not been made to low fat, low sugar choices
- You may experience dumping syndrome which occurs if you eat too much sugar, fat or alcohol, or large amounts of food—it is not considered a health risk, but can be very unpleasant with symptoms including nausea, vomiting, diarrhoea, sweating, faintness, weakness and increased heart rate
- Nausea and vomiting may occur, particularly in the first few days after surgery—vomiting is also common if you eat too quickly or eat too much

