Bariatric dietetics
After your Bariatric Surgery
Surgical wound closure
Depending on your surgeon you may have wound closure in a number of ways. If you have surgical staples or non-absorbable sutures they will need to be removed at your GP 10 days after surgery. If you have absorbable sutures you may remove your dressing after 5-7 days and the sutures will dissolve/ absorb themselves. Please check with the ward nurse which would closure you have before discharge.
Bathing
Getting your wound wet is not recommended for the first week as this may cause infection. The dressing can be changed after 5 days of discharge. If there is any oozing, redness or swelling please see your practice nurse. Once the wounds are healed you can shower but we do not recommend you take a bath for 14 days after surgery.
Pain
We advise that you take pain killers you are given. If you find they are not helping with the pain please contact your GP or the Clinical Nurse Specialist.
Physical activity/lifting
No strenuous or heavy lifting should be avoided for about 6 weeks. Lifting will put pressure on your wound which needs time to heal.
Sexual activity
You may resume your normal sexual activity as soon as it feels comfortable for you.
Eating and drinking
You have been given post-surgery dietary leaflets; you are advised to adhere to them strictly.
Time off work
We recommend you take 2 weeks off work after surgery. If you have a manual job this may need to be increased or you may need to negotiate restricted duties. Please ensure that you ask the staff on ward to arrange your sick certificate before you are discharged.
Driving
Driving should not be attempted for 2 weeks or until you feel confident that you are able to perform an emergency stop. Please check with your insurance regarding policy on abdominal surgery.
Dietary Guidance after Intra-gastric Balloon Insertion
Introduction
The intra-gastric balloon is a soft silicone balloon that is placed inside the stomach and filled with saline (sterile water) and some blue dye. By taking up space within your stomach, the balloon helps you feel full from a smaller amount of food. Together with a balanced diet and increased physical activity levels an intra-gastric balloon can help you lose weight.
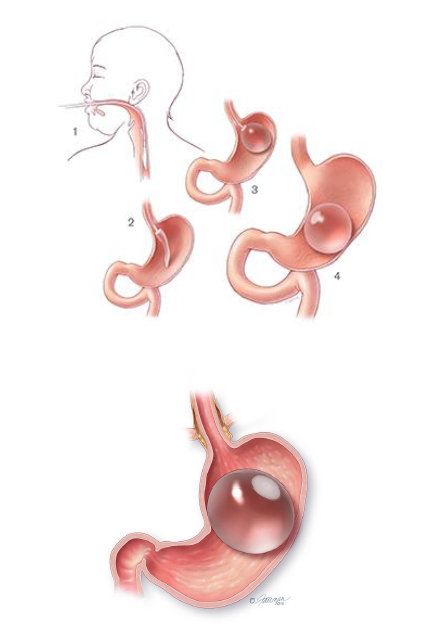
What happens during intra-gastric balloon insertion?
The balloon will be inserted through a tube down your throat either under light sedation, or under general anaesthetic. The tube will not interfere with your breathing at any time as it passes down your oesophagus not into your wind pipe.
Once in your stomach the balloon is inflated with saline and some blue dye. The volume of saline inserted varies from 500–700mls. Once inflated, the balloon is too large to pass into the bowel and it will float freely inside the stomach. The procedure generally takes 20–30 minutes.
How long does the balloon stay in place?
The balloon can remain inside for 6 to 12 months. Longer periods of use are not recommended as over the time the acid content of the stomach will weaken the balloon material and cause the balloon to deflate.
How much weight will I lose with the balloon?
The amount of weight you lose can vary but on average people lose up to 20kg through balloon, diet and physical activity.
Do I need to follow a specific diet prior to balloon insertion?
Your stomach must be completely empty prior to balloon insertion.
Therefore, you must stop eating for at least 6 hours, and drink any liquids for 4 hours, before the procedure.
If you are required to take any specific medication at a specific time then you are advised to consult to your GP or bariatric team for further advice.
Do I need to follow a specific diet prior to balloon removal?
For intragastric balloon removal, it is necessary to follow a clear liquid only diet for 3 days prior to your scheduled procedure date.
During this time you should consume a clear liquid diet consisting of only the following:
- Water
- Black tea or black coffee (no sugar)
- Broth
- Vegetable juice (no pulp)
- Squash (no added sugar)
Post-operative Diet
This information will guide you through the post- operative stages step-by- step after gastric band insertion.
The texture progression phases from fluids to solids are important to reduce the risk of unpleasant side effects such as nausea, vomiting, pain and discomfort. Therefore it is important not to skip any of the stages.
You will need to follow a modified texture diet for 2 weeks, before returning to a regular texture diet. The diet is separated into 4 separate stages:
- Liquids
- Puree
- Soft
- Regular
Stage 1 – only smooth liquids for 1 week (day 0-7)
You can start to take sips of fluids as soon as you feel able to. To get the most success from the balloon you must wait about 20–30 minutes after eating before having a drink—this will also help to wash any food debris that may have become stuck to the balloon. Remember to sit upright during and after meals. Drink small quantities throughout the day—do not allow yourself to become too thirsty as you will not be able to drink large quantities at a time. Start with sips (little and often), and if you feel comfortable then gradually increase the amount.
- Avoid fizzy/carbonated drinks and alcohol
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
- All liquids should be completely smooth with no bits or lumps (e.g. can be sucked through a straw).
- Avoid big gulps as this may cause discomfort, nausea, sickness and regurgitation.
Which liquids are suitable?
- Skimmed or semi-skimmed milk or lacto-free or soya milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes
- SlimFast or alternative meal replacement shake
- Low-fat natural or plain yoghurt drinks
- Complan soup
- Meritene soup
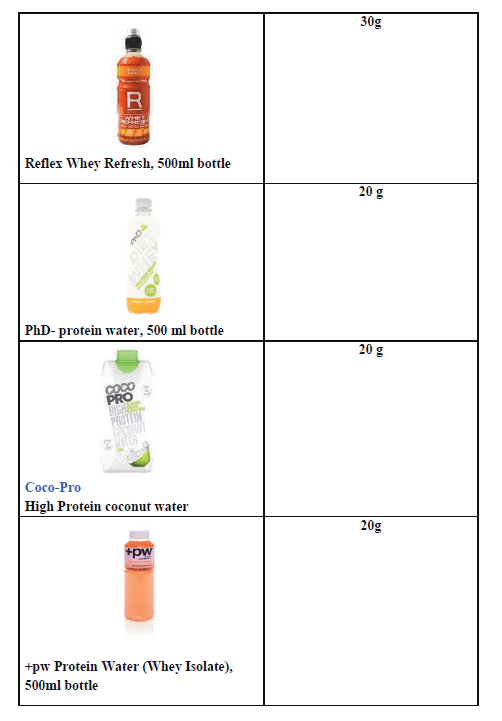
- Protein Water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Sample meal plan
- Breakfast: High protein shake
- Lunch: SlimFast shake or Meritene/Complan soup (1 sachet)
- Evening meal: High protein shake or Meritene/Complan Soup
- Snacks in between meals: if you feel hungry in between meals you can consume 200ml of skimmed/semi-skimmed/lacto-free/soya milk 8
Stage 2 – only puree foods for 4 days (day 8-11)
All food during this stage should be pureed and completely smooth with no bits or lumps.
Puree foods are smooth and can pass through your stomach easily. You must use a blender, liquidiser or a food processor to puree your food to the correct consistency. Aim for a smooth consistency like ‘yoghurt’.
Try to include foods that are high in protein in your meals to keep you fuller for longer.
How much and when?
Eat 5-6 small meals throughout the day during this stage. Start with 1-2 tablespoons at your meals and snacks, and if you feel comfortable gradually increase the amount.
As you progress through the puree stage, you may find that your portions gradually increase. However, remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
- Avoid fizzy/carbonated/sugary drinks and alcohol.
Which foods are suitable?
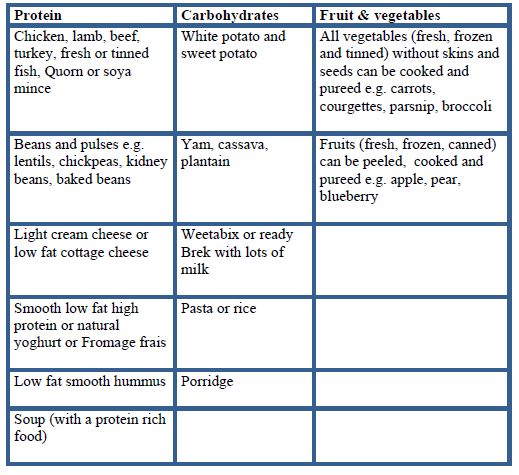
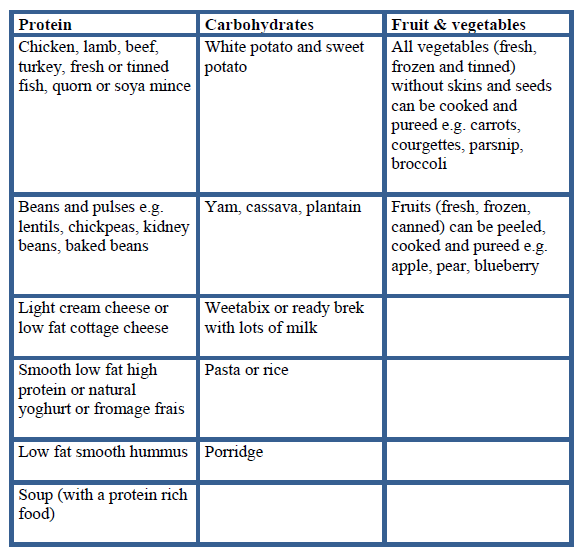
All of the foods in the table below are suitable, and will need to be pureed.
Sample meal plan
Breakfast:
Weetabix, Oatibix OR Ready Brek with plenty of skimmed/semi-skimmed/lacto-free/soya milk OR high protein yogurt pot or pouch
Lunch and Dinner ideas:
- Puree chicken with potato and vegetables
- Puree spaghetti bolognaise and vegetables
- Puree lentil or vegetable or chicken soup
- Puree tinned fish (tuna, sardines, and mackerel) with potato and vegetables
- Puree baked beans/tinned chickpeas.
Snacks:
Low-fat yogurt (with no bits), low-fat humous, low-fat custard with pureed fruit, smoothie (with no bits), home-made milkshake (with no bits, healthy recipe)
Stage 3 – soft, fork-mashable foods for 3 days (day 12-14)
Soft foods are foods that have a soft consistency, are well cooked that can easily be mashed with a fork. You do not need to use a blender during the soft stage.
Foods to avoid:
Avoid any foods that are hard or contain skins, seeds and pips as these will be difficult to mash into a soft consistency
- Sweet corn, peas, celery, fresh tomato, potato skin, nuts, seeds, hard cheese
- Dry, crumbly foods e.g. biscuits, crackers
- Food that has a mixed consistency e.g. minestrone soup, cereal flakes with milk
- Avoid fizzy/carbonated/sugary drinks and alcohol
How much and when?
Eat 3 meals a day and if you feel hungry between your meals, then have a snack. Use a small plate for your main meals, ¾ of your plate should include a protein and vegetables, and the remaining ¼ of your plate should include carbohydrates. Remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
Sample meal plan
Breakfast ideas:
- Porridge, Oatibix or Weetabix with skimmed milk
- Mashed baked beans
- Soft cooked eggs e.g. scrambled, poached, omelette
Lunch and Dinner ideas:
- Tinned or soft flaky fish with mashed potato and vegetables
- Shepherd’s pie or cottage pie with mashed vegetables
- Minced chicken/beef/lamb/turkey with couscous/mashed potato and vegetables
- Minced quorn or soya mince with pasta and vegetable
- Omelette with low fat grated cheese with mashed, peeled, seedless tomato
- Cauliflower cheese
- Risotto with soft mashed vegetables
- Chicken or meat casserole
- Thick soups e.g. lentil, ham, leek and potato
- Chicken/fish/beef/lamb/vegetable stews
Snack ideas:
200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder) or high protein shake or high protein yoghurt or low fat custard or low fat yoghurt
Stage 4 – Regular foods from day 15 and onwards
From day 15 and onwards you can gradually introduce regular texture foods and increase the variety of foods in your diet.
Continue to eat 3 regular meals each day and try not to leave more than 3-4 hours between meals.

- EAT FIRST -Protein (meat, fish, poultry, eggs, beans, pulses)
- EAT SECOND- Vegetables and salad
- EAT LAST - Carbohydrates (bread, rice, potato, pasta, grains)
Eating Guidance
- You should not graze (eat small amounts of food constantly through the day) or go for a long-period of time without eating.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated. Avoid having large quantities at atime.
- Limit alcohol intake, you are allowed to have 1 or 2 glasses of alcoholic beverage on social occasions only.
- Avoid high fat, high calorie foods, snacks and sugary drinks as these will not assist with weight loss.
- Aim to eat slowly, chew thoroughly, separate eating and drinking.
- Aim to have a drink 30minutes after you have finished eating to ‘rinse’ the balloon
- Use a side plate to help guide your portions and follow the plate model below.
- If you are hungry in-between meals then choose a nutritious snack such as a piece of fruit, high protein yoghurt, handful of mixed nuts or a glass of skimmed/semi skimmed/soya/lacto-free milk.
Possible problem foods
There may be foods after an intra-gastric balloon insertion that some people find difficult to tolerate and feel like they get ‘stuck’ or may make you sick. These include; firm or dry red and white meat, bread, rice and pasta.
Possible Side Effects:
There can be some side effects to having the balloon inserted; the most common ones are listed below:
Nausea and vomiting
Nausea and vomiting are very common after the procedure. You will be given anti-sickness medication to help control this. It is common however, to have these symptoms for a couple of weeks after the procedure as your stomach adjusts to the balloon being in place.
To help with nausea make sure you are chewing your food thoroughly, separate eating and drinking and consume small portions.
Try moving around even if you don’t feel like it, as it will help the food to move from the stomach into the gut.
If you are struggling to keep any fluids down after the first four days or if you are concerned, please contact the hospital team.
Reduced stool volumes or reduced frequency of bowel movements
This is common and normally relates to the smaller amount of food being eaten. Normal bowel movements can be anything from 3 times per day to 3 times per week.
If your stool is hard to pass, make sure you are drinking enough water throughout the day (most people need about 2 litres per day). You should also aim to include fibre foods in your diet such as fruit, vegetables and wholegrain cereals/breads. These foods will help to relieve constipation and also tend to be low in calories and filling.
Heartburn and acid reflux
Heartburn and acid reflux are common after balloon insertion and medication will be prescribed to help control this. Some foods, such as caffeine, alcohol, spicy and fatty foods, can make reflux worse, if taken in large quantities.
Small amounts of low-fat milk and dairy products can help with acid reflux as can staying upright after meals and stopping eating at least 2 hours before going to bed.
You will be given some medication while you are in hospital (usually lansoprazole) to reduce stomach acid and prevent stomach ulcers forming. You will be given a small supply of this medication to take home with you when you are discharged. It is essential that you continue to take this medication for the whole time you have the balloon in place. Please make sure to contact your GP for a repeat prescription once the hospital supply has finished.
Odour associated with belching/burping
Bad –smelling belching or burping can be a problem and is likely related to food getting stuck in and around the mucous that coats the balloon. To avoid this, ensure you have a drink 30 minutes after eating, chew your food well and try to move around a lot as this can help stop the food from getting stuck.
Bloating
This is common and is caused by the balloon sitting in the stomach. Unfortunately there is little that can be done for this other than to have the balloon removed. Try to remember that although bloating can be uncomfortable the balloon is only temporary and is there to help you reduce your weight. If you are unable to tolerate the discomfort from bloating the balloon will need to be removed.
What happens if the balloon deflates spontaneously?
If the balloon deflates before a scheduled removal you should notice blue dye in your urine or stools. Contact the team and come to our A&E Department immediately so we can remove the balloon.
Vitamins and minerals
Due to the reduced portion sizes and overall food intake, you will not get adequate vitamins and minerals from the diet. Therefore you will need to start taking an additional vitamin and mineral supplementation once daily. As soon as you are able to start having liquids, you can begin taking your multivitamin and mineral supplement.
Dietary Guidance after Gastric Band Surgery
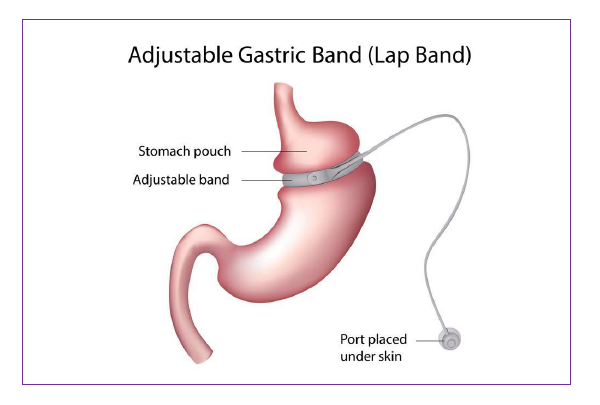
Introduction
This information will guide you through the post- operative stages step-by- step following insertion of a gastric band.
The texture progression phases from fluids to solids are important to reduce the risk of unpleasant side effects such as nausea, vomiting, pain and discomfort. The gradual texture progression also helps to avoid damage to your new stomach, allows your wounds to heal after surgery and allows food to pass easily from the stomach to your small intestine. It is important not to skip any of the stages.
You will need to follow a modified texture diet for 4 weeks, before returning to a regular texture diet. The diet is separated into 4 separate stages:
- Liquids
- Puree
- Soft
- Regular
The day after your surgery, your surgical team will tell you when it is safe for you to begin to sip fluids. A member of the dietetic team will see you before you go home to discuss the post-operative diet and answer any questions you may have.
Stage 1 – only smooth liquids for 1 week
All liquids should be completely smooth with no bits or lumps (e.g. can be sucked through a straw). Start with sips (little and often), and if you feel comfortable then gradually increase the amount. Avoid big gulps as this may cause discomfort, nausea, sickness and regurgitation.
Choose liquids that are high in protein to:
- help with wound healing and quicker recover
- prevent muscle loss
- keep you fuller for longer.
During this stage aim to have 1.5-2 litres of fluids each day to stay hydrated.
It is advisable to prioritise protein rich fluids over others such as tea, coffee etc.
Begin with sipping your drinks little and often and gradually increase the quantity until the sensation of feeling full occurs.
It is important to stop as soon as you feel full. If you drink too much, your stomach may overfill and cause pain, nausea and vomiting.
Which liquids are suitable?
Choose protein rich liquids at least 1 litre (2 pints) each day to help your body recover such as:
- Skimmed or semi-skimmed milk or lacto-free or soya milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes
- Slimfast shake
- Low-fat natural or plain yoghurt drinks
- Complan soup
- Meritene soup
- Protein Water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Fluids to avoid:
- Fruit juices, malt drinks and fruit smoothie’s with bits
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Sample meal plan
Breakfast: High protein shake
Lunch: Slimfast shake or Meritine/Complan soup (1 sachet)
Evening meal: High protein shake or Meritene/Complan Soup
Snacks in between meals: if you feel hungry in between meals you can consume 200ml of skimmed/semi-skimmed/lacto-free/soya milk with or without the addition of 1 tablespoon of skimmed milk powder.
Stage 2 – only puree foods for 1 week
All food during this stage should be pureed and completely smooth with no bits or lumps.
Puree foods are smooth and can pass through your stomach easily. You will need to use a blender, liquidiser or food processor to puree your food to the correct consistency. Aim for a smooth consistency like ‘yoghurt’.
Include foods that are high in protein in your meals to keep you fuller for longer, and also prevent muscle loss.
How much and when?
Eat 5-6 small meals throughout the day during this stage. Start with 1-2 tablespoons at your meals and snacks, and if you feel comfortable gradually increase the amount. As you progress through the puree stage, you may find that your portions gradually increase. However, remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
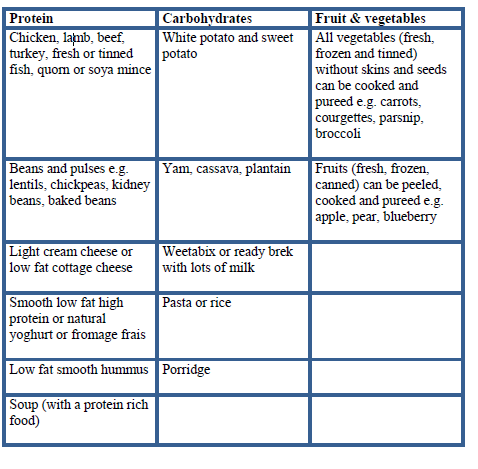
Which foods are suitable?
The main focus for your meals and snacks is protein so always eat this first. All of the foods in the table below will need to be pureed. Foods from other food groups such as carbohydrates, fruit and vegetables are also suitable, but are not a rich source of protein. If you choose to eat these then add some extra protein such as; protein or skimmed milk powder, high protein yoghurt, skimmed milk or low fat cheese to fortify them.
Foods to avoid:
Any food not pureed with a blender, liquidiser or food processor.
Suitable fluids:
- Skimmed/Semi-skimmed milk/Soya/Lacto-free milk
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
- Smooth fruit smoothies made with milk or skimmed milk powder.
Aim to drink 1.5-2 litres of fluids each day.
Fluids to avoid:
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Sample meal plan
Breakfast: Weetabix, Oatibix or Ready Brek with plenty of skimmed milk OR high protein yogurt pot or pouch
Lunch and Dinner ideas:
- Puree chicken with potato and vegetables
- Puree spaghetti bolognaise and vegetables
- Puree lentil or vegetable or chicken soup
- Puree tinned fish (tuna, sardines, mackerel) with potato and vegetables
Half your meal portion should be from a protein rich food. Try adding 2tsp of protein or skimmed milk powder to your puree foods.
Snacks: aim for 2-3 across the day: 200ml glass of skimmed milk (add 1-2tsp of skimmed milk powder) or protein shake or high protein yoghurt
Stage 3 – soft, fork-mashable foods for 2 weeks
Once you have completed the puree stage you can move onto soft foods. It is important to follow this stage as your stomach is still healing and recovering from surgery.
What is soft food?
Soft foods are foods that have a soft consistency, are well cooked and can be easily mashed with a fork. You do not need to use a blender during the soft stage.
Foods to avoid:
Any foods that are hard or contain skins, seeds and pips as these will be difficult to mash into a soft consistency
- Sweet corn, peas, celery, fresh tomato, potato skin, nuts, seeds, hard cheese
- Dry, crumbly foods e.g. biscuits, crackers
- Food that has a mixed consistency e.g. minestrone soup, cereal flakes with milk
How much and when?
Eat 3 meals each day and if you feel hungry between your meals, then have a snack. Use a side plate for your main meals, and fill ½ of your plate with protein rich foods. Start with 3-4tbsp at meal times and stop eating at the first signs of fullness or if you feel uncomfortable. Remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
What foods are suitable?
The main focus for your meals and snacks is protein, so continue to eat this first.
Sample meal plan
Breakfast ideas:
- Porridge, Oatibix or Weetabix with skimmed milk
- Mashed baked beans
- Soft cooked eggs e.g. scrambled, poached, omelette
Lunch and Dinner ideas:
- Tinned or soft flaky fish with mashed potato and vegetables
- Shepherd’s pie or cottage pie with mashed vegetables
- Minced chicken/beef/lamb/turkey with couscous/mashed potato and vegetables
- Minced quorn or soya mince with pasta and vegetable
- Omelette with low fat grated cheese with mashed, peeled, seedless tomato
- Cauliflower cheese
- Risotto with soft mashed vegetables
- Chicken or meat casserole
- Thick soups e.g. lentil, ham, leek and potato
Snack ideas:
- 200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder) or high protein yoghurt or low fat custard or low fat yoghurt
Suitable fluids:
- Skimmed/Semi-skimmed milk/Soya/Lacto-free milk
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
- Smooth fruit smoothies made with milk or skimmed milk powder.
Aim to drink 1.5-2 litres of fluids each day.
Fluids to avoid:
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Stage 4 – regular foods from week 5 onwards
From week 4 after surgery your stomach should have healed enough for you to gradually introduce regular texture foods and increase the variety of foods in your diet.
Continue to eat 3 regular meals each day and try not to leave more than 3-4 hours between meals. You should not graze (eat small amounts of food constantly through the day) or go for a long-period of time without eating.
Use a side plate to help guide your portions and follow the plate model below, so that you are always prioritising protein first. If you are hungry in-between meals then choose a nutritious snack such as a piece of fruit, high protein yoghurt or a glass of skimmed/semi skimmed milk.

EAT FIRST: Protein (meat, fish, poultry, eggs, beans, pulses)
EAT SECOND: Vegetables and salad
EAT LAST: Carbohydrates (bread, rice, potato, pasta, grains)
There may be foods after a gastric band insertion that some people find difficult to tolerate and feel like they get ‘stuck’ or may make you sick. These include; chewy or dry red and white meat, bread, fibrous fruit and vegetables, rice, pasta, nuts and seeds. Avoid these at the beginning of the regular stage (stage 4) and then re-introduce them gradually once a ‘regular’ diet has been established.
What shall I do if food gets stuck?
If this happens it may be because you have eaten a food that was too solid, eaten too quickly or too much, or because of eating certain ‘problem’ foods. This will feel uncomfortable and you may wretch or vomit. Often it will resolve itself, however you could try drinking a small amount of cold sparkling water, as the fizz may help to dislodge the food that is stuck.
What else can you expect after surgery?
Side effects
Vomiting
After your surgery vomiting can occur. It is often the result of:
- Eating too much
- Eating too quickly
- Not chewing your food well enough
- Eating and drinking together, or too closely together
- Eating foods that are not the correct consistency for the stage you are in
- If you continue to vomit after checking the above and you are still within the first 2 months after surgery, you could try returning to the puree or liquid phase for a short period to see if your symptoms improve.
- If you continue to vomit and the cause cannot be explained then please contact your surgeon or GP.
Constipation
You may experience constipation during texture progression stages due to reduced fibre intake. If you experience constipation make sure you are drinking enough fluids. You should aim for 1.5-2 litres of fluids each day. During the early post-operative stages it can be difficult to get enough fibre as your focus is on protein. When you are in the puree stage, include some puree cereals and fruit and vegetables in your diet to help your bowels work more efficiently. If constipation persists then speak to your GP about a suitable laxative.
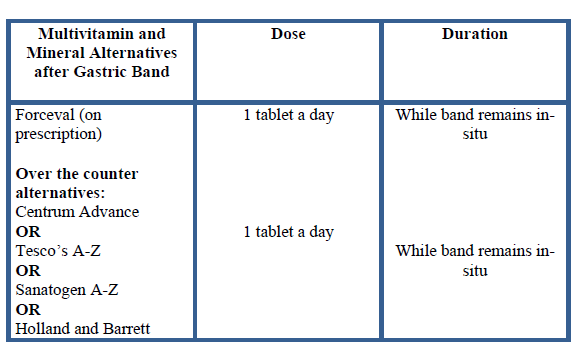
Vitamins and minerals
Due to the reduced portion sizes and overall food intake, you will not get adequate vitamins and minerals from the diet. Therefore you will need to start taking an additional vitamin and mineral supplementation once daily. As soon as you are able to start having liquids, you can begin taking your multivitamin and mineral supplement.
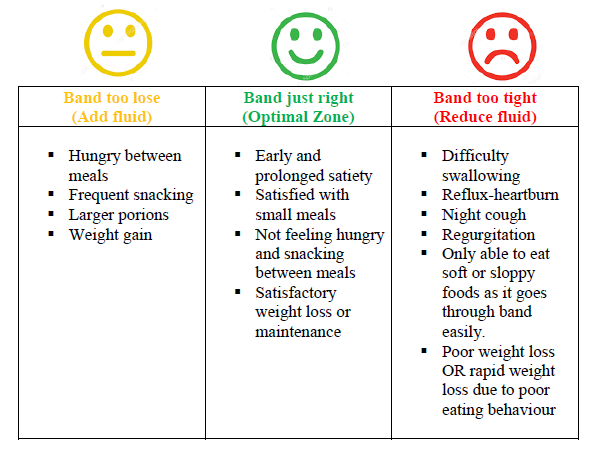
Gastric Band Adjustments:
Your first appointment for a gastric band adjustment will be 6-8 weeks following surgery. This fill is usually done under X-ray and the position of your band will also be checked at this time. Further band fills can be arranged through the bariatric nurse specialist in band clinic in outpatients or, under X-ray.
Prior to your first band fill you may start to feel hungry. This is because the band is usually empty and the swelling around the band from surgery that originally caused some feeling of restriction has reduced. It is very important that you follow the ‘golden rules’ (see the last page) and eat healthily to avoid weight gain prior to your first band fill.
There are some indications that show whether the band is too loose, too tight or band is just right. The table below shows these indications. Please be aware; if the band is too tight, you may either lose weight due to not being able to keep anything down or you may gain weight because you can only tolerate liquid or very sloppy foods which may be higher in calories.
Dietary goals for successful weight loss after bariatric surgery ‘The Golden Rules’
- Eat 3 small regular meals each day, avoid long periods of fasting
- Do not ‘graze’
- Plan snacks if you get hungry between meals
- Use a side plate to portion your meals
- Eat protein foods first
- Eat slowly: put a small amount of food in your mouth at a time (size of a thumbnail) and chew this very well (at least 20 times). Take 20-30 minutes to complete your meal
- Eat at a table or without any distractions and try putting your cutlery down between mouthfuls
- Do not eat until you are ‘full’. Overeating will stretch your stomach pouch, cause discomfort and may cause vomiting
- Do not drink with meals. Drink 20 minutes before meals and then wait at least 20 minutes after a meal before you drink some fluids
- Aim to drink at least 1.5-2 litres of fluid a day
- Avoid all alcohol
- Avoid all fizzy drinks as these can cause discomfort, bloating and stretch your small stomach pouch
- Avoid high calorie drinks such as smoothies, fruit juice, energy drinks and milkshakes as they contain a lot of sugar (and therefore calories) and can affect your weight loss following surgery
Seven simple pre operation meal ideas
Meal Ideas
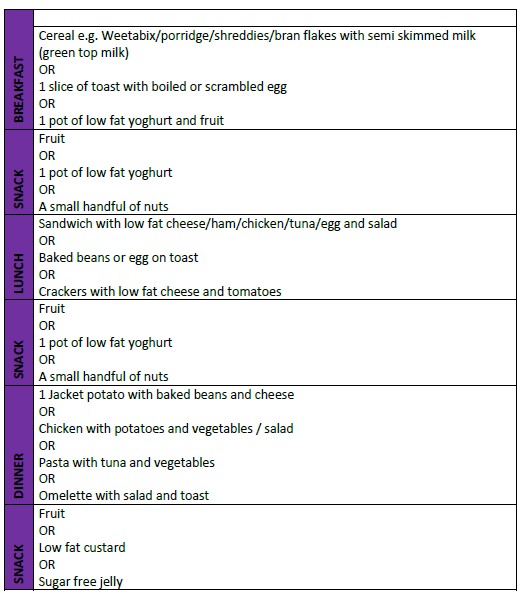
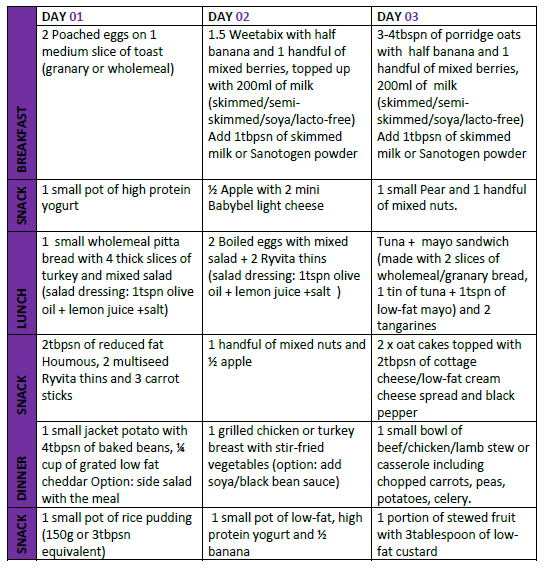
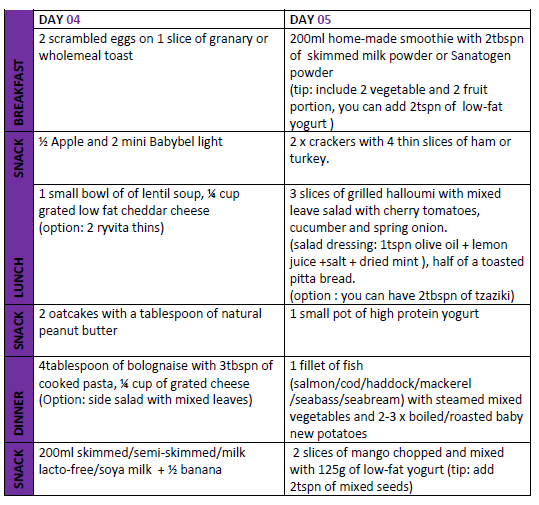
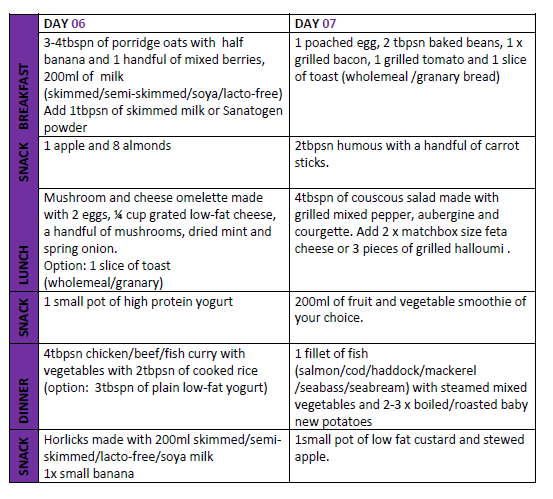
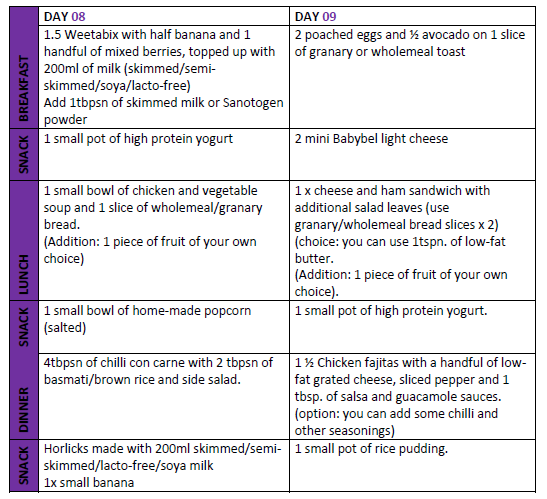
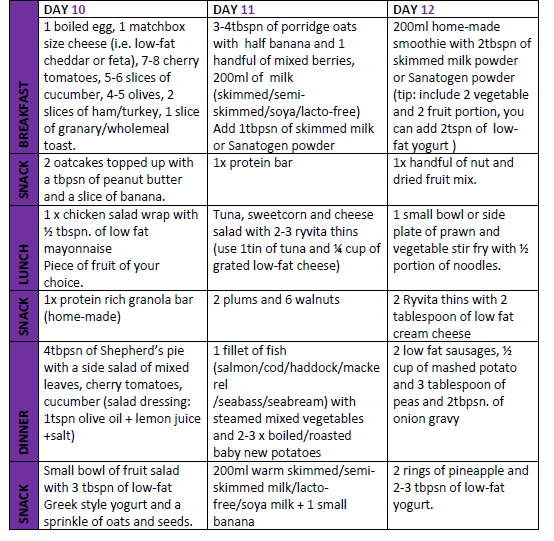
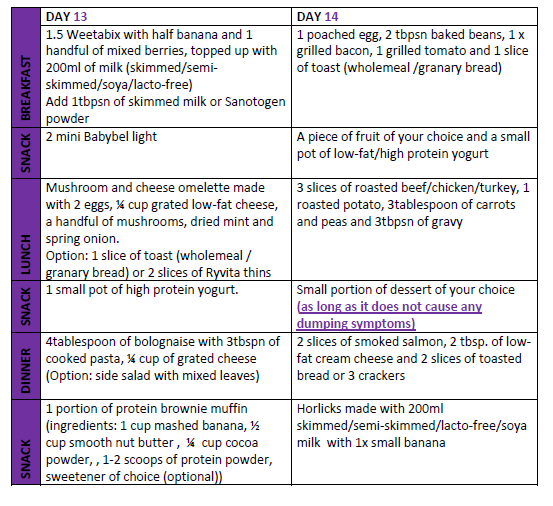
Fourteen day post operation meal ideas
Meal Plan
Dietary Guidance after Gastric Bypass or Sleeve Gastrectomy Surgery
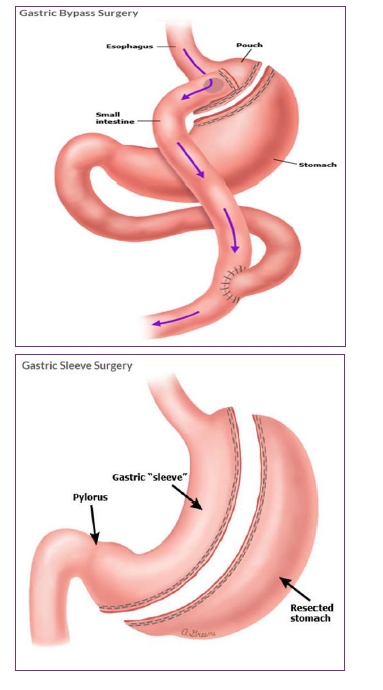
Introduction
This information will guide you through the post- operative stages step-by- step after gastric bypass or sleeve gastrectomy surgery.
The texture progression phases from fluids to solids are important to reduce the risk of unpleasant side effects such as nausea, vomiting, pain and discomfort. The gradual texture progression also helps to avoid damage to your new stomach, allows your wounds to heal after surgery and allows food to pass easily from the stomach to your small intestine. It is important not to skip any of the stages.
You will need to follow a modified texture diet for 6 weeks, before returning to a regular texture diet. The diet is separated into 4 separate stages:
- Liquids
- Puree
- Soft
- Regular
The day after your surgery, your surgical team will tell you when it is safe for you to begin to sip fluids. A member of the dietetic team will see you before you go home to discuss the post-operative diet and answer any questions you may have.
Stage 1 – only smooth liquids for 2 weeks
All liquids should be completely smooth with no bits or lumps. Start with sips (little and often), and if you feel comfortable then gradually increase the amount. Avoid big gulps as this may cause discomfort, nausea, sickness and regurgitation.
Choose liquids that are high in protein to help you to meet your protein requirements. The average recommendation is 70-100g each day. Aim to have 1.5-2 litres of fluids each day to stay hydrated.
Always prioritise protein rich fluids over others such as tea, coffee etc. Begin with sipping your drinks little and often and gradually increase the quantity until the sensation of feeling full occurs. It is important to stop as soon as you feel full. If you drink too much, your stomach may overfill and cause pain, nausea and vomiting.
Which liquids are suitable?
Choose protein rich liquids at least 1 litre (2 pints) each day to help your body recover such as:
- Skimmed or semi-skimmed milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes
- Slimfast
- Low-fat natural or plain yoghurt drinks
- Complan soup
- Meritene soup
- Protein Water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Fluids to avoid:
- Fruit juices, malt drinks and fruit smoothies
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Sample meal plan
Breakfast: High protein shake
Snack: 200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder)
Lunch: Slimfast
Snack: Meritine soup (1 sachet)
Evening meal: High protein shake
Snack: 200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder)
How much and when?
Try to have 1.5-2 litres of fluids each day. Aim for at least 1litre (2 pints) of milk based fluids (see list of protein rich fluids above) and always prioritise protein rich fluids over others such as tea, coffee etc. Begin with sipping your drinks little and often and gradually increase the quantity until the sensation of feeling full occurs. It is important to stop as soon as you feel full. If you drink too much, your stomach may overfill and cause pain, nausea and vomiting.
Stage 2 – only puree foods for 2 weeks
All food during this stage should be pureed and completely smooth with no bits or lumps.
It is important to complete this stage as your stomach pouch will be very small and tight at first. Puree foods are smooth and can pass through your stomach easily. You will need to use a blender, liquidiser or food processor to puree your food to the correct consistency. Aim for a smooth consistency like ‘yoghurt’.
Choose foods that are high in protein to help you to meet your protein requirements (at least 70g protein each day). Aiming for at least 500ml (1 pint) of protein rich fluids daily will help you achieve this.
How much and when?
Eat 3 meals and 3 snacks each day. Start with 1-2 tablespoons at your meals and snacks, and if you feel comfortable gradually increase the amount. As you progress through the puree stage, you may find that your portions gradually increase. However, remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
Which foods are suitable?
The main focus for your meals and snacks is protein so always eat this first. All of the foods in the table below will need to be pureed. Foods from other food groups such as carbohydrates, fruit and vegetables are also suitable, but are not a rich source of protein. If you choose to eat these then add some extra protein such as; protein or skimmed milk powder, high protein yoghurt, skimmed milk or low fat cheese to fortify them.
Foods to avoid:
Any food not pureed with a blender, liquidiser or food processor.
Suitable fluids:
Try to choose protein rich liquids in between your meals:
- Skimmed or semi-skimmed milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes, protein water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Fluids to avoid:
- Fruit juices, malt drinks and fruit smoothies
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Aim to drink 1.5-2 litres of fluids each day.
Sample meal plan
Breakfast: Weetabix, Oatibix or Ready Brek with plenty of skimmed milk OR high protein yogurt pot or pouch
Lunch and Dinner ideas:
- Puree chicken with potato and vegetables
- Puree spaghetti bolognaise and vegetables
- Puree lentil and vegetable soup
- Puree tinned fish (tuna, sardines, mackerel) with potato and vegetables
Half your meal portion should be from a protein rich food. Try adding 2tsp of protein or skimmed milk powder to your puree foods
Snacks: aim for 2-3 across the day: 200ml glass of skimmed milk (add 1-2tsp of skimmed milk powder) or protein shake or high protein yoghurt
Stage 3 – only soft foods for 2 weeks
Once you have completed the puree stage you can move onto soft foods. It is important to follow this stage as your stomach is still healing and recovering from surgery.
What is soft food?
Soft foods are foods that have a soft consistency, are well cooked and can be easily mashed with a fork. You do not need to use a blender during the soft stage.
Foods to avoid:
Any foods that are hard or contain skins, seeds and pips as these will be difficult to mash into a soft consistency
- Sweet corn, peas, celery, fresh tomato, potato skin, nuts, seeds, hard cheese
- Dry, crumbly foods e.g. biscuits, crackers
- Food that has a mixed consistency e.g. minestrone soup, cereal flakes with milk
How much and when?
Eat 3 meals each day and if you feel hungry between your meals, then have a snack. Use a side plate for your main meals, and fill ½ of your plate with protein rich foods. Start with 3-4tbsp at meal times and stop eating at the first signs of fullness or if you feel uncomfortable. Remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
What foods are suitable?
The main focus for your meals and snacks is protein, so continue to eat this first.
Sample meal plan
Breakfast ideas:
- Porridge, Oatibix or Weetabix with skimmed milk
- Mashed baked beans
- Soft cooked eggs e.g. scrambled, poached, omelette
Lunch and Dinner ideas:
- Tinned or soft flaky fish with mashed potato and vegetables
- Shepherd’s pie or cottage pie with mashed vegetables
- Minced chicken/beef/lamb/turkey with couscous/mashed potato and vegetables
- Minced quorn or soya mince with pasta and vegetable
- Omelette with low fat grated cheese with mashed, peeled, seedless tomato
- Cauliflower cheese
- Risotto with soft mashed vegetables
- Chicken or meat casserole
- Thick soups e.g. lentil, ham, leek and potato
Snack ideas:
200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder) or high protein shake or high protein yoghurt or low fat custard or low fat yoghurt
Suitable fluids:
Try to choose protein rich liquids in between your meals:
- Skimmed or semi-skimmed milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes, protein water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Fluids to avoid:
- Fruit juices, malt drinks and fruit smoothies
- Fizzy drinks (including fizzy water) as the gases may cause bloating, pain and can increase your stomach size
- All alcohol
Aim to drink 1.5-2 litres of fluids each day.
Stage 4 – regular foods from week 7 onwards
You will now have completed 6 weeks of texture progression and your stomach should have healed enough for you to gradually introduce regular texture foods and begin to increase the variety of foods in your diet.
Continue to eat 3 regular meals each day and try not to leave more than 4-5 hours between meals. You should not graze (eat small amounts of food constantly through the day) or go for a long-period of time without eating.
Use a side plate to help guide your portions and follow the plate model below, so that you are always prioritising protein first. If you are hungry in-between meals then choose a nutritious snack such as a piece of fruit, high protein yoghurt or a glass of skimmed milk.

EAT FIRST:
- Protein (meat, fish, poultry, eggs, beans, pulses)
EAT SECOND:
- Vegetables and salad
EAT LAST:
- Carbohydrates (bread, rice, potato, pasta, grains)
Possible problem foods
There may be foods after a bypass or sleeve that some people find difficult to tolerate and feel like they get ‘stuck’ or may make you sick. These include; chewy or dry red and white meat, bread, fibrous fruit and vegetables, rice, pasta, nuts and seeds. Avoid these at the beginning of the regular stage (stage 4) and then re-introduce them gradually once a ‘regular’ diet has been established.
What shall I do if food gets stuck?
If this happens it may be because you have eaten a food that was too solid, eaten too quickly or too much, or because of eating certain ‘problem’ foods. This will feel uncomfortable and you may wretch or vomit. Often it will resolve itself, however you could try drinking a small amount of cold sparkling water, as the fizz may help to dislodge the food that is stuck.
What else can you expect after surgery?
Side effects
Vomiting
After your surgery vomiting can occur. It is often the result of:
- Eating too much
- Eating too quickly
- Not chewing your food well enough
- Eating and drinking together, or too closely together
- Eating foods that are not the correct consistency for the stage you are in
- If you continue to vomit after checking the above and you are still within the first 2 months after surgery, you could try returning to the puree or liquid phase for a short period to see if your symptoms improve.
- If you continue to vomit and the cause cannot be explained then please contact your surgeon or GP. Very occasionally there may be a narrowing where the new joins in your intestine have been created and this may require a procedure to stretch the area, so that food can move through.
Dumping syndrome
After surgery, avoid food and drinks high in sugar and fat. If these are taken even in small amounts, they can cause ‘Dumping Syndrome’. The symptoms are:
- Nausea
- Sweating
- Abdominal cramps
- Palpitations (rapid heart rate)
- Diarrhoea
- Dizziness
- Feeling faint
Dumping syndrome occurs when fatty or sugary foods are emptied or ‘dumped’ from the stomach into the small intestine too rapidly. It is usually easy to identify dumping syndrome and the food or drink that has triggered it, as symptoms usually occur within 30-60 minutes after consumption. If you experience dumping syndrome then try to sit or lie down until your symptoms improve. In the long term avoiding fatty and sugary food will help you manage dumping syndrome, as well as helping you to achieve your weight loss goal.
Hair loss
During the first 6-9 months after your surgery, you will experience rapid weight loss and hair loss can occur. By following a healthy balanced diet with enough protein and taking your vitamin and mineral supplements, should result in your hair returning to normal.
Constipation
If you experience constipation make sure you are drinking enough fluids. You should aim for 1.5-2 litres of fluids each day. During the early post-operative stages it can be difficult to get enough fibre as your focus is on protein. When you are in the puree stage, include some puree cereals and fruit and vegetables in your diet to help your bowels work more efficiently. If constipation persists then speak to your GP about a suitable laxative.
Reactive Hypoglycaemia
Reactive hypoglycaemia (low blood glucose) is a recognised complication after surgery and is the result of the alteration in your intestine, hormonal changes and the way you digest carbohydrates (sugars). The symptoms are:
- Sweating
- Palpitations (rapid heart rate)
- Feeling shaky
- Dizziness
- Feeling faint
- Confusion
- Weakness
The symptoms of reactive hypoglycaemia usually occur within 1-4 hours after a meal. If you think you are experiencing reactive hypoglycaemia then contact one the bariatric dietitians for advice, as reactive hypoglycaemia can often be managed with dietary changes. Keeping a food and symptom diary can be helpful to identify foods that trigger symptoms. If dietary changes do not help you to manage reactive hypoglycaemia, then the dietitian will refer you to endocrinology for further investigations and advice.
Hunger and appetite
In the early post-operative period you may not feel hungry because of your smaller stomach and the changes in gut hormones that will affect your appetite. It is still important to eat 3 regular meals and snacks (if needed), with the main focus on your protein intake.
A regular meal pattern with your smaller stomach can be a challenge and with less feelings of hunger, you may be tempted to skip meals thinking that this may speed your weight loss. However this can result in you becoming malnourished and deficient in protein and vitamins and minerals. Skipping your meals may also encourage unhelpful eating behaviours such as snacking / grazing that in the long term may result in weight regain.
Vitamins and minerals
After surgery reduced food intake may increase your risk of vitamin and mineral deficiencies. Daily, life-long vitamin and mineral supplementation is essential.
As soon as you are able to start having liquids, you can begin taking your multivitamins and minerals. During this stage some vitamins and minerals will be soluble. Once you move through the texture stages your GP can prescribe you with a tablet or chewable form.
Remember to space your vitamins and minerals across the day, as taking them all together will affect how well you absorb them. You will need to take your calcium supplement separately from your multivitamins and minerals and iron.
Dietary goals for successful weight loss after bariatric surgery ‘The Golden Rules’
- Eat 3 small regular meals each day, avoid long periods of fasting
- Do not ‘graze’
- Plan snacks if you get hungry between meals
- Use a side plate to portion your meals
- Eat protein foods first
- Eat slowly: put a small amount of food in your mouth at a time (size of a thumbnail) and chew this very well (at least 20 times). Take 20-30 minutes to complete your meal
- Eat at a table or without any distractions and try putting your cutlery down between mouthfuls
- Do not eat until you are ‘full’. Overeating will stretch your stomach pouch, cause discomfort and may cause vomiting
- Do not drink with meals. Drink 20 minutes before meals and then wait at least 20 minutes after a meal before you drink some fluids
- Aim to drink at least 1.5-2 litres of fluid a day
- Avoid all alcohol
- Avoid all fizzy drinks as these can cause discomfort, bloating and stretch your small stomach pouch
- Avoid high calorie drinks such as smoothies, fruit juice, energy drinks and milkshakes as they contain a lot of sugar (and therefore calories) and can affect your weight loss following surgery
Liver shrinkage diet for Bariatric Surgery

Introduction
What is the purpose of a liver shrinkage diet?
Liver shrinkage diet (LRD) is a diet based on low energy (calories), in particular low in carbohydrate and fat.
By following a liver shrinkage diet, your body will be forced to use up the stored carbohydrate (glycogen) from the liver. The glycogen and a quantity of water will leave the liver, and therefore liver will shrink and become softer, more flexible and easier to move during surgery.
During laparoscopic (keyhole) surgery the liver has to be lifted out of the way to access the stomach lying beneath it. Most people needing bariatric surgery have a large, fatty liver which can cause difficulty for keyhole surgery.
A large, fatty liver makes it harder for the surgeon to see and gain access to the stomach underneath. This can increase the duration of your surgery and therefore your time under general anaesthetic.
It can also be dangerous as your liver could bleed heavily during surgery or there could be injury to other organs. If this happens the surgeon may have to do open surgery instead of keyhole surgery.
If you do not follow the liver shrinkage diet and your liver has not shrunk, surgery may be deemed unsafe and the surgeon may cancel the surgery on the day.
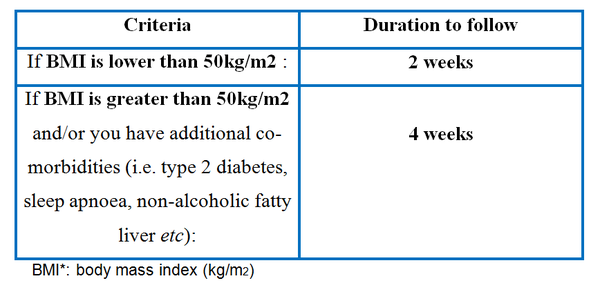
How long will I have to follow the liver shrinkage diet?
Duration of the diet is based on below criteria:
What are the liver shrinkage diet options?
OPTION 1 - SlimFast Meal Replacement Diet
OPTION 2 - Milk and Yogurt Diet
OPTION 3 - Food based Diet
All of the above diets are designed to provide:
- Around 800-1000kcal
- Less than 100g of carbohydrate
- Low fat
- High protein
You are required to pick one of the options and follow it as per instructions. Please do not mix different diet options as it will not show effective results.
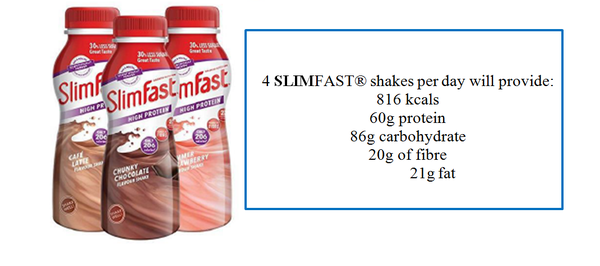
OPTION 1 – SLIMFAST® MEAL REPLACEMENT DIET
SLIMFAST® is a nutritionally complete, low calorie diet (LCD) meal replacement product. With this diet you are required to have:
- 4x 325ml (pre-made) SLIMFAST® bottles per day.
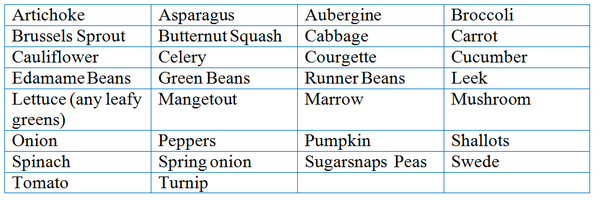
- 2 x cereal bowls of salad/vegetables from the list provided below: (cooking method: blended into soup/boiled/steamed/roasted/raw)
How can you make your meal interesting?
- Season your food: Add herbs, chilli, spices, garlic, salt and pepper freely
- Skip the ready-made dressings: Avoid adding any oil or salad dressings.
Lemon juice and vinegar (including balsamic vinegar) is allowed.
- Keep hydrated: Aim to have at least 2 litres of fluids per day including: water, sugar free squash, herbal tea, black tea, black coffee (no sugar).
- You are allowed to have 1 salty drink a day to help maintaining electrolyte levels.For example: 2 teaspoons of Stock or Marmite or Bovril or Consommé dissolved in a large glass of warm water.
Please note you are NOT ALLOWED to have the powdered version of SlimFast as it is high in calories and carbohydrate.
OPTION 2 – MILK AND YOGURT DIET
This diet is purely based on milk, yogurt and additional fluids only.
Alcohol and all other food sources should be avoided for the period of this diet.
Daily intake:
- 3 pints of skimmed OR semi skimmed milk OR lacto-free OR soya milk per day. The milk can be hot/cold and flavoured with vanilla essence, SUGAR FREE syrups (e.g. Crusha, Monin).
- 2 x 125g low-fat plain or natural yogurt or 0% fat yogurt per day. Aim to avoid fruit yogurts as they can be high in sugar and fat. You can add sugar free syrups or flavourings into the plain/natural yogurt to adjust the taste if needed.
- An additional minimum of 2litres of fluid per day (i.e. water, calorie free or low calorie squash/flavoured water, tea/coffee, fruit/herbal teas)
- Avoid adding any sugar into your tea/coffee. Sweeteners are allowed to be used as an alternative. You can use milk from your daily allowance to add into your tea or coffee.
- You will need to take supplements daily as this diet is not nutritionally complete. For example: Sanatogen A-Z, Tesco’s A-Z, Centrum Advance/Performance, Holland and Barrett.
- You are allowed to have 1 or 2 salty drink a day to help maintaining electrolyte levels. For example: 2 teaspoons of Stock or Marmite or Bovril or Consommé dissolved in a large glass of warm water.
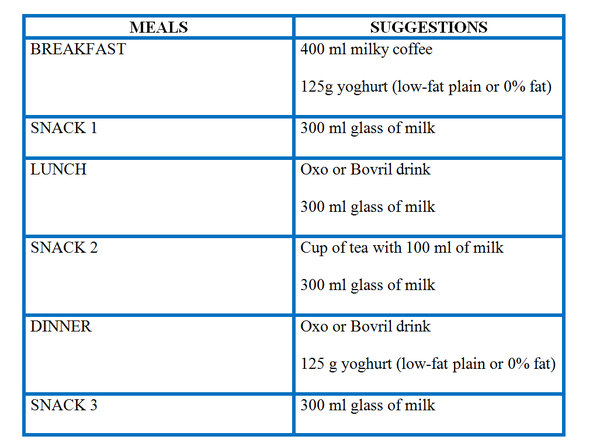
EXAMPLE OF A MEAL PLAN
OPTION 3 – FOOD BASED DIET
This diet is based on low carbohydrate, low energy, low fat and moderate protein meals and additional fluids throughout the day.
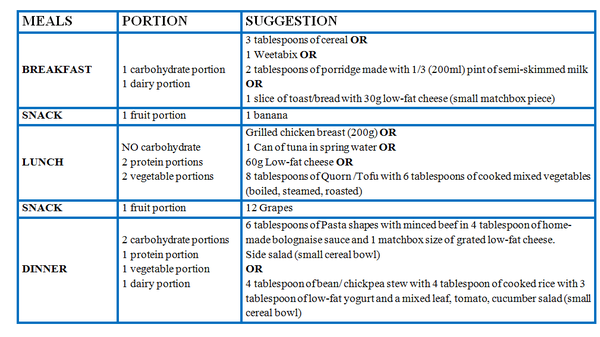
Your meals should follow the below format:
Breakfast:
- 1 carbohydrate portion
- 1 dairy portion
Lunch:
- NO carbohydrate
- 2 protein portions
- 2 vegetable portions
Evening:
- 2 carbohydrate portions
- 1 protein portion
- 1 vegetable portion
- 1 dairy portion
Snacks:
- 2x pieces of fruit per day - can be taken anytime
What is a portion?

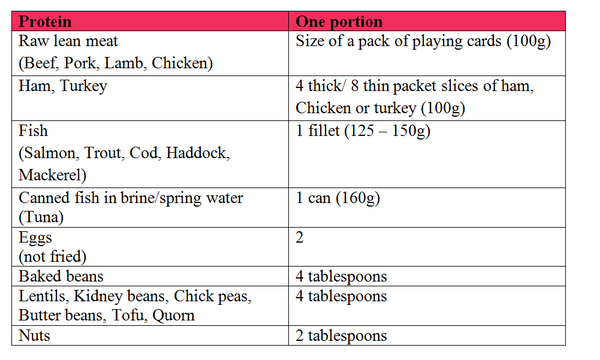
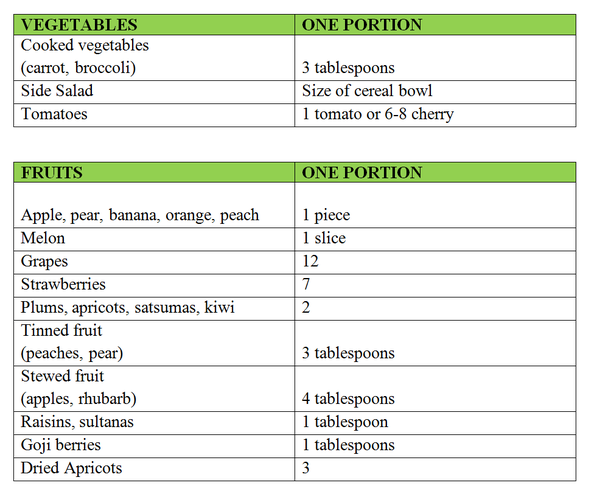
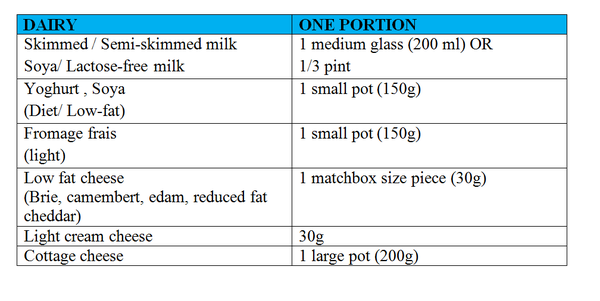
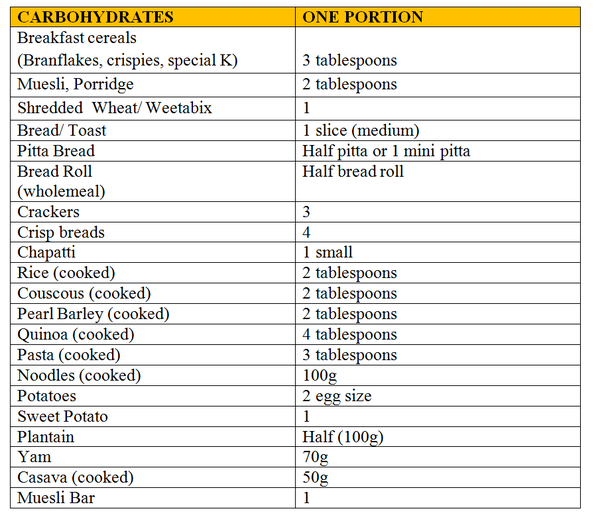
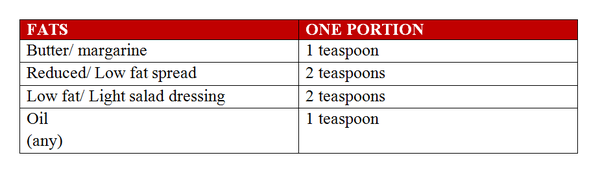
Example of a meal plan:
Foods to avoid:
It is important you avoid any foods high in sugar and fat, this includes:
- Sweets
- Chocolate/cakes
- Jelly
- Ice cream
- Sugary drinks including juices/fizzy drinks
- Alcohol
- Sugar added to hot drinks/ food (sweeteners are allowed to be used as alternative).
- Crisps
- Fried foods/ takeaways
- Creamy or ready-made pasta or meal sauces (choose tinned tomatoes to use in cooking i.e. in bolognaise sauces/stews/casseroles).
- Meat/fish products that have breadcrumbs (choose the fresh / lean options)
Fluids:
Minimum of 2L of fluids including:
- Water
- Tea/Coffee (you can add milk from your daily dairy allowance – see above)
- Sugar free squash/ sugar free flavoured water
You will need to start taking a multivitamin and mineral supplementation once daily as this diet is not nutritionally complete. For example: Sanatogen A-Z, Tesco’s A-Z, Centrum Advance/Performance, Holland and Barrett.
Additional Information
- You may experience headaches or feel “light-headed” after starting the liver shrinkage diet; this is quite usual and will pass in the first few days.
- Constipation can become a problem when following this diet because it contains very little fibre. You may need to take 1-2 sachets of Fybogel each day or any other laxatives in the tablet or powder form in order to prevent this. We do not recommend taking Lactulose during pre-op liver shrinkage diet.
- Patients on insulin or gliclazide (tablets): If you have diabetes and take insulin injections or gliclazide (tablets) please contact the person who normally helps you control your diabetes. It is likely you will need to reduce your insulin or gliclazide because the diets are all low in carbohydrate (less than 100g) and will make your blood sugars go lower than normal. Check your blood glucose levels 4 times a day. If you do not have a blood meter, you can ask to have your blood sugar checked at your local pharmacy. Please contact to your dietitian if you experience regular hypo’s (low blood sugar levels).
- It is expected that you experience some weight loss during liver shrinkage diet. Therefore; female patients need to be aware that you may experience a change in your menstrual cycle during this period. Additionally, women with PCOS (polycystic ovary syndrome) may ovulate and become fertile while on liver shrinkage diet, therefore it is important to use contraception.
- Please note you need to stop any food consumption 6 hours prior to your surgery and you are only allowed to have water up to 2 hours prior to your surgery.
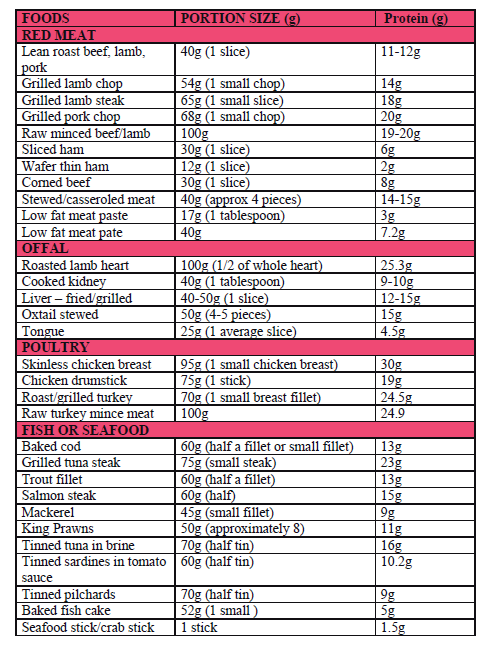
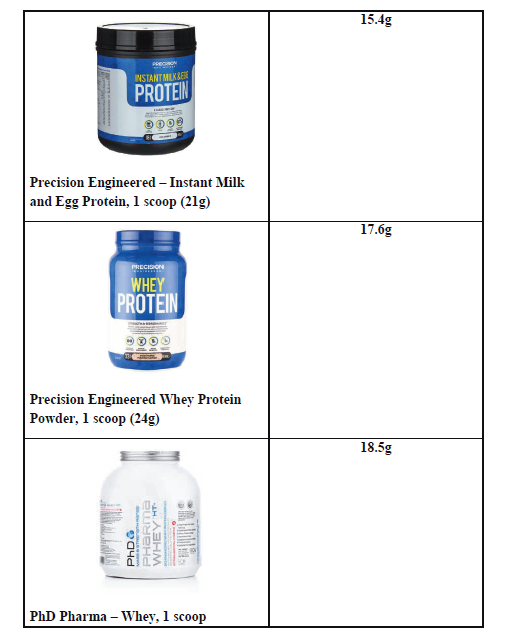
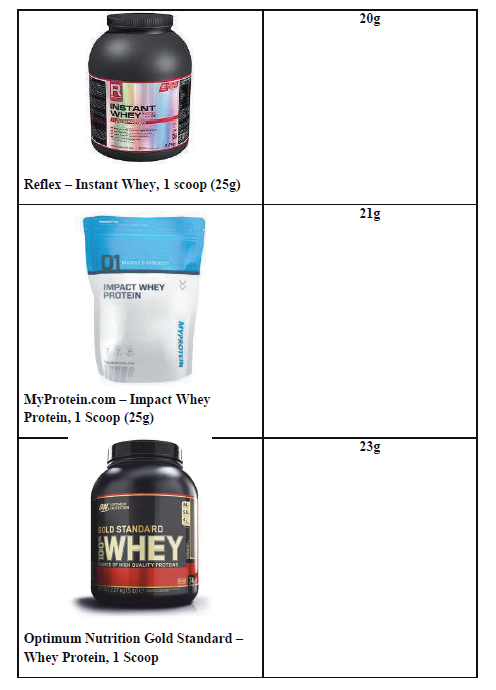
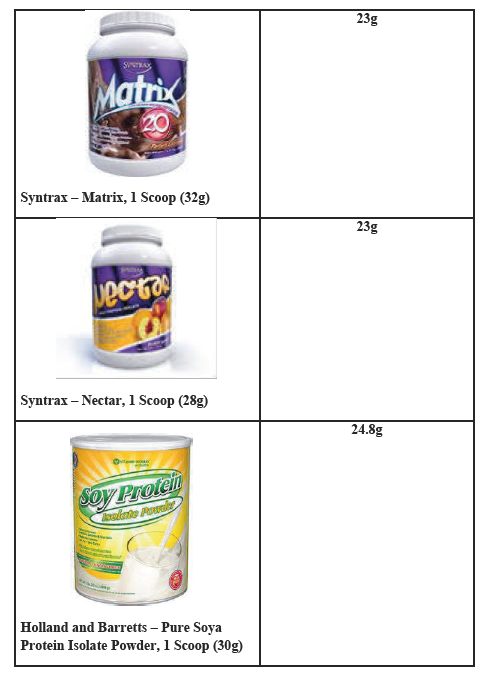
Protein after Bariatric Surgery
This information booklet is designed to provide you with more understanding in importance of protein rich foods in your diet after bariatric surgery.
Why is protein important to have in my diet?
Protein is important as it is:
- Essential building-block for the body
- Necessary for growth and repair
- Important in helping to fight infections.
After bariatric surgery, it is important to have a protein rich food at each meal time.
Ideally you should aim to have 70-100 grams of protein a day.
Good sources of protein include:
- Red meat, poultry, fish
- Eggs
- Beans and pulses
- Dairy foods (e.g. milk, cheese, yoghurt)
- Non-dairy alternatives (eg. soya based dairy, lacto free)
- Tofu and Quorn
These foods are also good sources of some essential vitamins and minerals.
- Vitamins A, B, and D
- Minerals: Iron and Zinc
Top Tips:
- Plan your menu in advance; base your meals and snacks around foods that are high in protein.
- Choose low-fat varieties or lean meat; cut any visible fat off. Avoid adding fat when cooking these foods.
- Chew meat, chicken and fish well before you swallow to avoid it getting stuck.
- Eat slowly.
- You may find roasted meats more difficult to tolerate. If this is the case then you may find alternative ways to cook meats which may be easier, for example, stewed meats, casseroled meats, slow cooked meat, minced meat, and wafer thin meats.
“Aim to eat protein rich food of your meal first”

- EAT FIRST: Protein (meat, fish, poultry, eggs, beans, pulses)
- EAT SECOND: Vegetables and salad
- EAT LAST: Carbohydrates (bread, rice, potato, pasta, grains)
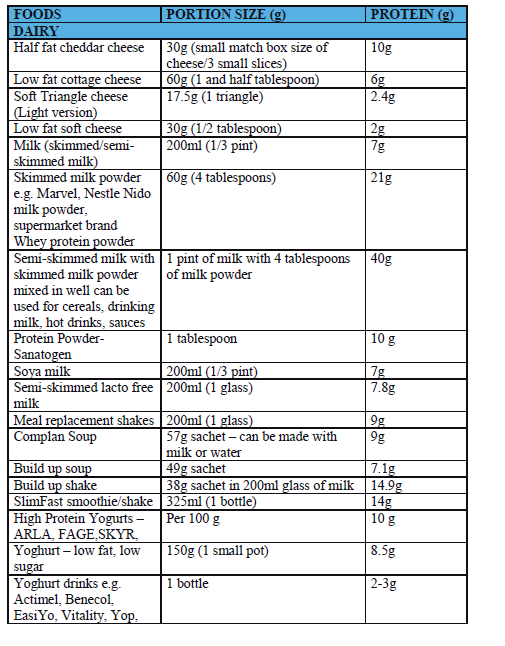
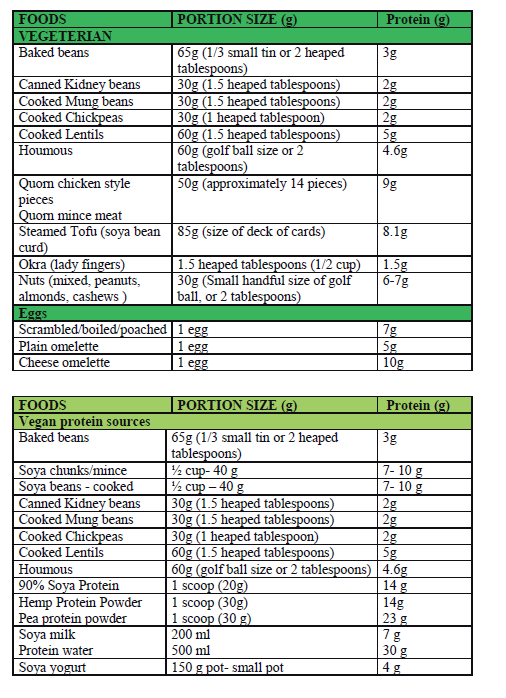
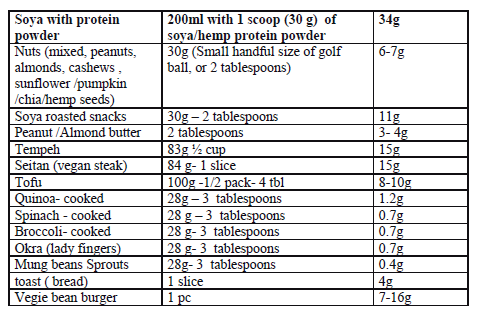
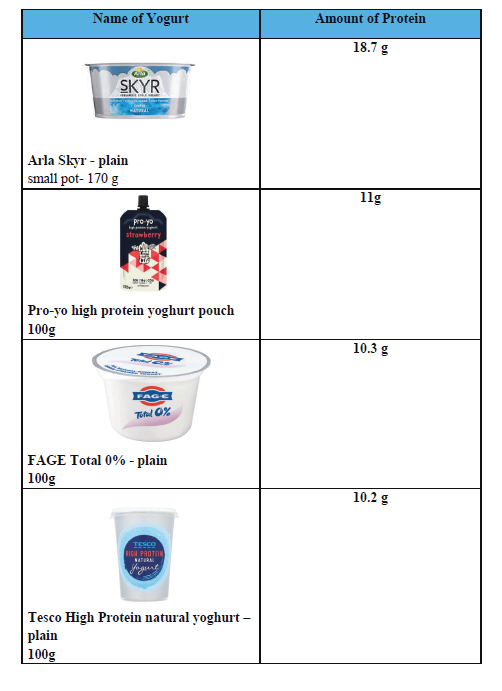
Amount of protein in foods
The following tables show the amount of protein per potion in detail.
Protein supplementaion and Bariatric Surgery
After bariatric surgery it can be difficult to meet your requirements for protein as food intake is very small. You need adequate protein as your ability to absorb protein is not as efficient as it was before surgery.
- Protein is essential for your body to heal and maintain muscle mass whilst you are losing weight.
- Ideally we would like you to aim to include at least 70g of protein in your diet each day.
Using a protein supplement can be a useful way to achieve this particularly in the first 6 months following your operation.
The ideal protein supplements are made from dairy protein (whey or casein protein), egg white protein, or soya protein. These are the most readily absorbed by your body and contain complete protein. A complete protein (or whole protein) is a source of protein that contains all 9 of the essential amino acids that are necessary to meet the dietary needs of humans in the correct proportions to support the functioning of the human body.
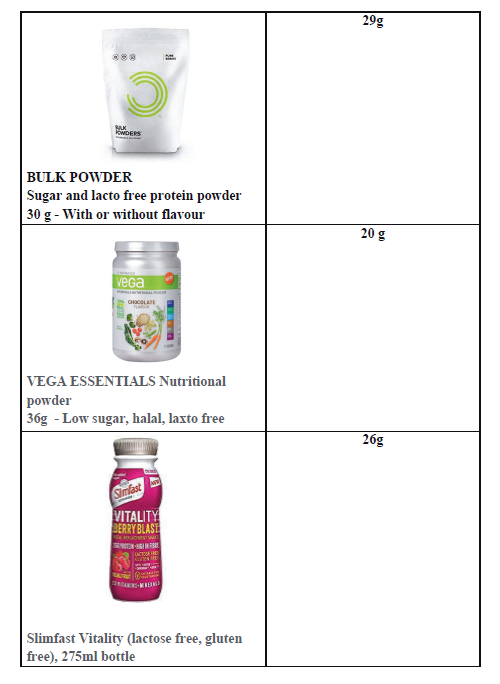
Below are some example protein supplements available that are low in calories, carbohydrate and fat, but high in protein. You may find others on the market; look for one that contains the least amount of calories for the most protein.
Whey protein powder is the most readily available protein supplement and can be found in many supermarkets and health food stores. Ideally they should be made with skimmed milk as it will further increase the protein content for the same volume of fluid.
Food Fortification
- Skimmed Milk Powder

Added into milk, this can be a useful tool in helping increase protein intake and be a cheaper alternative to protein shakes.
For example: 1 pint skimmed milk + 4 tablespoons of skimmed milk powder = 40g protein.
It can also be used in soups and other recipes.
- Sanatogen High Protein Powder (casein)

Flavourless powder to add into milk or food e.g. soups / stews / porridge.
Per 2 teaspoons = 5.5g protein
Effective way to add protein value of food without influencing flavour.
High protein yogurts
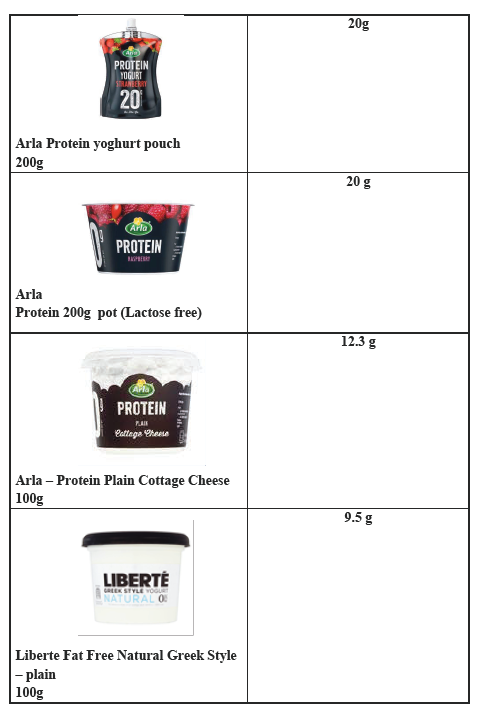
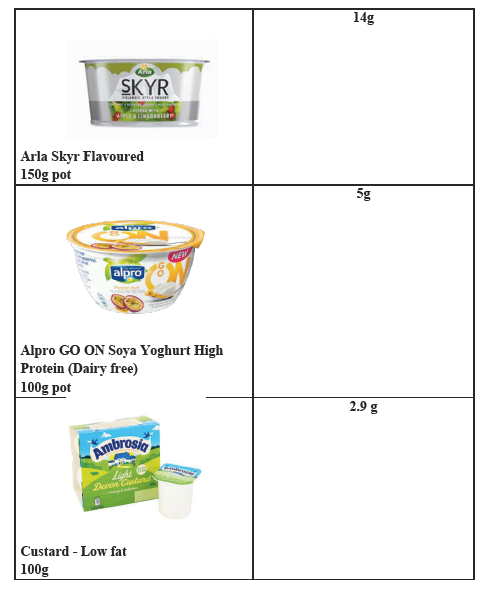
High protein supplements
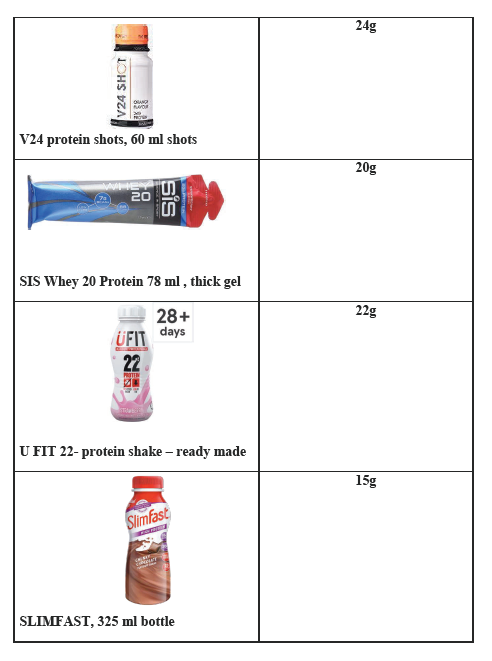
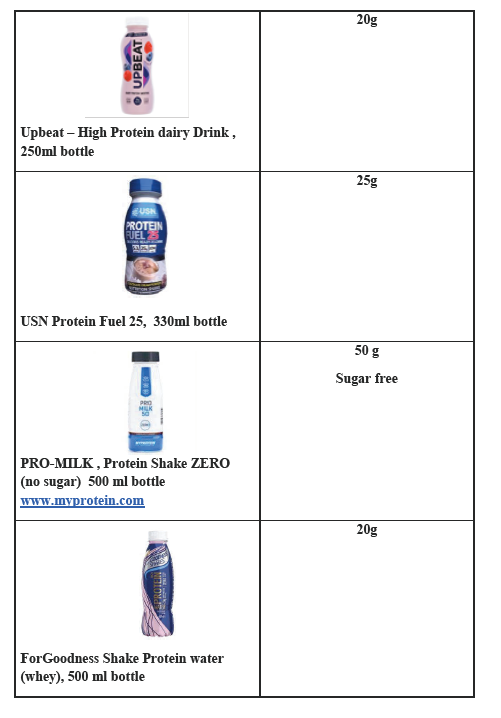
Protein Powders
Alternatives
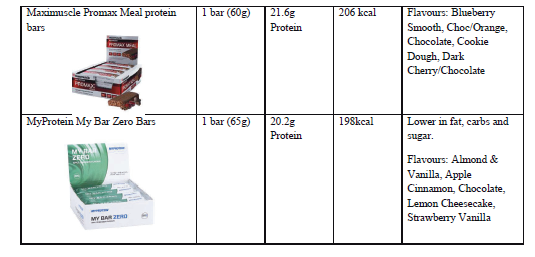
Protein bars (suitable for regular diet phase onwards only)
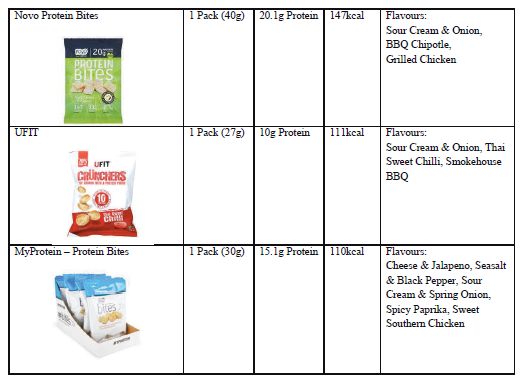
Protein Bites (suitable for those that can’t tolerate the drinks)
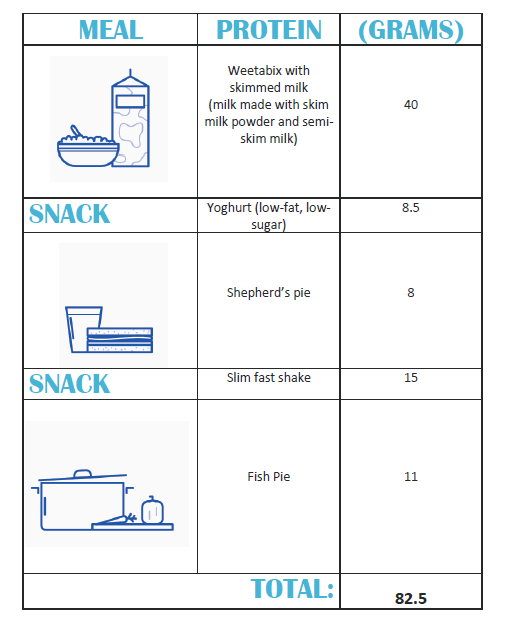
Protein challenge 70-100g daily

Example of a meal plan:
Ramadan and Fasting After Bariatric Surgery
During the Holy Month of Ramadan, patients who have undergone a bariatric surgery including gastric banding, sleeve gastrectomy and gastric bypass are required to take special measures to avoid health risks.
Patients are advised to not to fast in the first 12 – 18 months after bariatric surgery to prevent malnutrition and medical complications.
Patients who have had bariatric surgery may face some challenges during Ramadan period. These challenges could include:
- Altered eating behaviours and poor nutritional intake: Following bariatric surgery, patients are usually advised to have small, frequent meals, to eat slowly, chew thoroughly, to separate eating and drinking and stop when feeling satisfied. However, fasting for long periods could lead to the desire to consume larger quantities at a faster pace upon breaking the fast. This can result in abdominal discomfort, and nausea and vomiting leading to dehydration, malnutrition and possible vitamin and mineral deficiencies.
- Dehydration: It is advised that you drink at least 1.5-2L of fluids throughout the day following bariatric surgery to keep hydrated and help prevent constipation. Following bariatric surgery it is advised that you should not drink quickly, drink large amounts in one sitting or eat and drink together. These restrictions, together with fasting (especially during long summer days) can increase the risk of dehydration.
- Dumping Syndrome: Patients who have undergone a gastric bypass / sleeve gastrectomy surgery are more at risk of experiencing dumping syndrome and/or diarrhoea, due to the restricted meal pattern during fasting and consumption of traditional foods such as sugary desserts and deep-fried foods when breaking the fast.
- Vitamin and mineral deficiencies: Following bariatric surgery, patients are recommended to take regular vitamin and minerals by their specialist dietitians that need to be spaced out appropriately throughout the day. One of the challenges during Ramadan is that the reduced stomach capacity may make it difficult to have all of the recommended vitamins and minerals in a short time frame (dusk until dawn) and space them adequately, which may result in some deficiencies.
- Hypoglycaemia: The risk of hypoglycaemia (low blood glucose level) is increased when fasting for a significant period of time (i.e. more than 10 hours). For example, the length of time between Suhoor and Iftar.
Dietary and life-style recommendations for bariatric surgery patients during Ramadan
- Break the fast by choosing water, dried fruits including dates or soup to prepare your body for the main meal, which you should try to eat after Maghreb prayer. Beginning Iftar with water will help to overcome dehydration from fasting and having 1-2 dried dates will help to raise blood glucose levels after fasting for long hours (see example meal plan below).
- Ensure the main meal is composed of protein-rich food, vegetables/salad and slowly released carbohydrates. Remember the meal balance: aim to cover half of the plate with protein, and the remaining two quarters with vegetables and carbohydrates. Always start having the protein rich foods first then, vegetables and lastly carbohydrates.
- When you're fasting for long periods of time (i.e. more than 10hours), eating Suhoor early may result in hypoglycemia before Iftar. Therefore, in those circumstances take Suhoor as late as possible.
- Avoid sleeping directly after eating as this can lead to health problems such as acid reflux, abdominal discomfort and/or regurgitation.
- Remember the golden rules: eat slowly, chew thoroughly, separate eating and drinking, stop when you feel satisfied and avoid fizzy/sugary drinks.
- Avoid foods high in fat/sugar such as traditional desserts or deep-fried meals to avoid symptoms of dumping syndrome.
- Ensure good hydration; begin Iftar with 200-250ml of water. Aim to have at least 1.5L fluids per day.
- Continue to take vitamin and mineral supplements as per recommendations.
- Continue with your routine physical activities during Ramadan; however schedule them at appropriate times. For instance; exercise 2 hours after breaking the fast, then have a snack after for post-work-out recovery.
Example Meal Plan for Ramadan
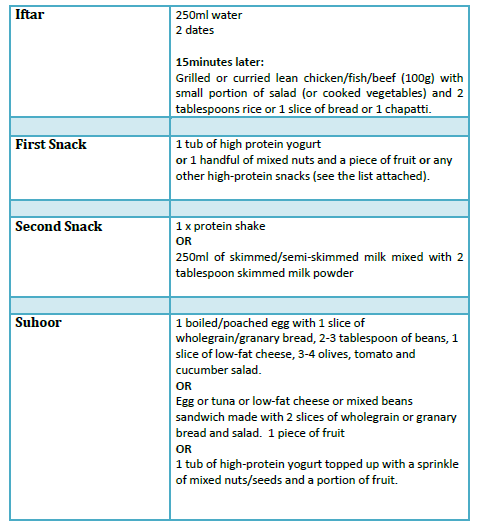
Throughout the day we advise you to keep yourself hydrated and aim to consume at least 1.5-2L of sugar free fluids.
Bari-Snack Alternatives
- Mixed nuts and dried fruit (closed handful)
- Sliced apple or celery with a tablespoon of natural peanut butter
- Two oat cakes topped with cottage cheese and black pepper
- 1 small pot of low-fat yoghurt and a portion of fruit
- 1 small pot of high protein yogurt
- Handful of carrot sticks with two tablespoons hummus
- 1-2 x Ryvita crackers topped up with oily fish e.g. pilchards/tuna/salmon flakes
- 5 x crab sticks
- 1 chicken drumstick
- 1 hard-boiled egg
- 2 x rice cakes topped up with 1 tablespoon of peanut butter
- Home-made fruit/vegetable smoothie (prepared with skimmed milk powder or protein powder)
- 1 x protein bar
- 1-2 mini babybell or cheese triangles
- 2 x slices of turkey
- Pumpkin seeds (closed handful)
- Low-fat yogurt drink
- 1 small bowl of mixed fruit salad
- 1 small bowl of salad with a matchbox size of feta cheese (add 2teaspoon of olive oil and lemon dressing)
- 250ml of skimmed/semi-skimmed milk mixed with 1-1.5tablespoon of skimmed milk powder (you can add sugar free flavourings)
Dessert alternatives: Sugar-free jelly, dried dates (no more than 3), low-fat custard and any other low-fat and low-sugar traditional dessert alternatives
Reactive Hypoglycaemia After Bariatric Surgery
What is Reactive Hypoglycaemia?
Reactive hypoglycaemia is the general term for hypoglycaemia (low blood glucose levels) after eating. It usually occurs a few hours after a meal, snack or drink (1-4 hours) and is a recognised complication after bariatric surgery.
What are the symptoms of reactive hypoglycaemia?
If these symptoms occur within 1-4 hours after eating, you may be experiencing reactive hypoglycaemia:
- Feeling sweaty
- Hungry
- Anxious
- Shaky
- Confusion
- Dizziness
- Difficulty coordinating movement S
- lurred speech
- Loss of consciousness
- Palpitations (rapid heart rate)
Why does reactive hypoglycaemia occur?
It is the result of the anatomical alterations to your gut and changes to gut hormones that occur after bariatric surgery and affect the way carbohydrates (sugars) are digested and absorbed. Reactive hypoglycaemia is closely linked to your diet and can often be managed with dietary changes.
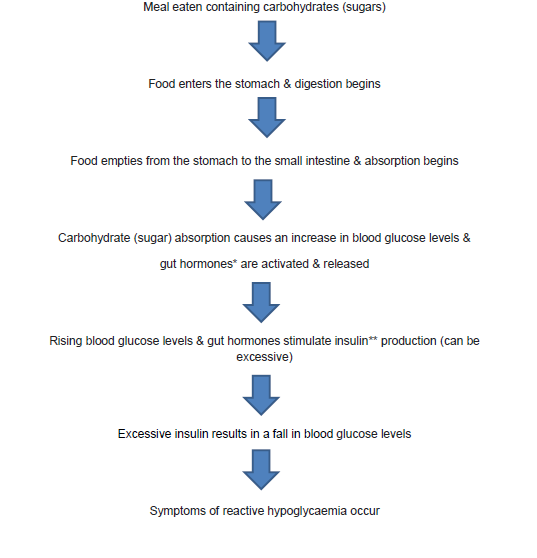
* Gut hormones: GLP 1 & Gastric inhibitory polypeptide
** Insulin is released in response to an increase in blood glucose levels. The role of insulin is to control blood glucose levels. It does this by signalling to the liver, muscle and fat cells to use glucose from the bloodstream for energy. If the body’s cells have enough energy then insulin signals to the liver to store the glucose as glycogen.
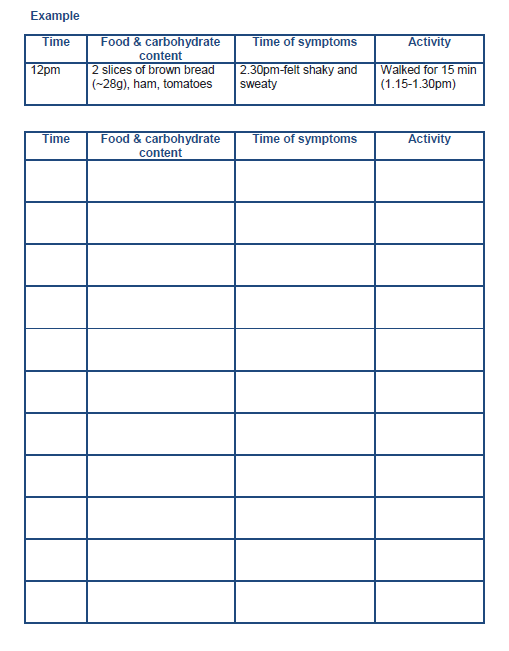
How is reactive hypoglycaemia diagnosed?
Keeping a food and symptom diary can be helpful to confirm (or not) whether any of the foods you eat are triggering symptoms. Record the type of food eaten, along with the amount and times of meals and symptoms using the diary in this booklet. This information can be shared with the Dietitian who can advise dietary changes to help improve your symptoms.
However, if the Dietitian is unable to help you manage your symptoms or your symptoms are severe, we will refer you to an Endocrinologist for further investigations and management.
Which Foods Contain Carbohydrate?
Carbohydrates can be divided into 2 groups; starchy (or complex) carbohydrates and free sugars.
Carbohydrates are found in; pasta, couscous, breakfast cereals, crackers, rice, fruit (fresh, tinned, dried), and starchy vegetables such as potatoes, yam and sweet potato. All of these are digested by your body to release glucose (sugar). Some processed foods that contain carbohydrates (free sugars) include; cakes and biscuits, sweets, chocolates, fruit juice and smoothies, jam, marmalade and honey.
Adapting your diet to manage reactive hypoglycaemia
The main principles:
- Eat small portions of food more regularly across the day
Ensure that meals and snacks are structured and spaced 3-4 hours apart so you do not have long gaps between eating. Eating 3 small meals and 2-3 snacks across the day can help to stabilise your blood glucose levels and avoid symptoms that may be caused by eating large portions of food (or carbohydrates).
- Try to limit your carbohydrates. Aim for 30g of carbohydrates at each main meal and 15g for snacks
Some studies have shown that limiting the amount of carbohydrates at mealtimes can help to avoid rapid rises in blood glucose levels after eating, excess insulin secretion and therefore avoid rapid drops in blood glucose levels that can result in the symptoms of reactive hypoglycaemia.
To begin with, it may be helpful to calculate the grams of carbohydrates you are currently having at mealtimes and if this amount causes symptoms then decrease it. For example, if you are having 2 thin slices of bread (around 20g carbohydrate) and this causes symptoms, then halve this to 1 slice (10g carbohydrate) to see if this prevents reactive hypoglycaemia. At the back of this booklet you will find a list of common foods with their average carbohydrate content, as well as other resources that you can use to calculate the carbohydrate content of food. Use the food and symptom diary to record the effects of any dietary changes.
- Choose Low Glycaemic Index carbohydrates
Carbohydrates are absorbed at different rates. Low Glycaemic Index (LGI) carbohydrates are digested and absorbed more slowly than High Glycaemic Index foods. Including a small amount of LGI carbohydrates at your meals may slow down the rise in blood glucose levels (after eating) and keep your blood glucose levels more stable afterwards. This may help to prevent (or reduce) symptoms of reactive hypoglycaemia. At the back of this booklet there is a list of some common LGI carbohydrates.
- Meet your protein recommendations (average of 70-100 grams/day)
Eat protein at all of your main meals and choose protein rich foods for snacks. Protein is important to preserve your muscle mass after surgery and it helps you to fill fuller for longer. Remember to prioritise protein, always eating this first during your meals or snacks.
- Eat more fibre
Fibre rich foods move more slowly from your stomach in to your small intestine. This can help to delay the increase in blood glucose levels after eating, decrease insulin secretion and therefore help to reduce the risk of reactive hypoglycaemia. Try to eat more fibre rich LGI foods such as oats, beans and pulses, granary bread, brown pasta, brown basmati rice and vegetables.
- Avoid eating and drinking together
Follow the ‘golden rules’ and separate eating and drinking. Avoid drinking less than 15 minutes before and wait 30 minutes after meals or snacks. Eating and drinking together can increase the rate at which food empties from your stomach into your small intestine that can cause a rapid rise in blood glucose levels and rapid secretion of insulin.
- Avoid sugary drinks
Avoid sugary drinks such as fruit juice, fizzy drinks, smoothies and milk shakes as these drinks are a source of carbohydrates (in liquid form) and are easily absorbed by the body. Sugary drinks can cause a rapid increase in blood glucose levels, as well as insulin and increase the risk of reactive hypoglycaemia. Suitable alternatives include; water, sugar free squash, tea, and coffee (with sweetener).
- Avoid alcohol
Alcohol can affect the way your liver produces and releases glucose so consumption may increase the risk of reactive hypoglycaemia. There is also some evidence that suggests an increased risk of alcohol dependency after bariatric surgery.
- Keep a food, symptom and activity diary
This can be useful and you can use it as a tool for reflection. Keeping a record of the times you eat, your symptoms and physical activity can help you identify triggers for your symptoms. In the long term if you are aware of your triggers, you can modify your diet to help you with managing your symptoms.
Treating severe symptoms of hypoglycaemia
If you experience severe symptoms of hypoglycaemia (confusion, difficulty coordinating, slurred speech) then you will need to administer some fast acting carbohydrate (in glucose form) to rapidly increase your blood glucose levels. The guidance suggests around 15 grams of glucose and some suitable options are:
- 3 Jelly babies
- 5 Glucotabs
- 5 Dextro energy tabs
- 4 Wine gums
- 175ml Lucozade energy (original)
- 60ml Lift Juice glucose shot
After 15-20 minutes of taking some fast acting carbohydrates your symptoms should begin to improve. You should then eat a small carbohydrate snack (if your next meal is not due). Opt for a LGI carbohydrate and some protein as this may help stabilise your blood glucose levels. A suitable option would be 1or 2 oat cakes (LGI) with some low fat cheese or a slice of cooked meat.
The purpose of treating hypoglycaemia is to rapidly increase your blood glucose level and reduce the risk of more severe symptoms of hypoglycaemia such as loss of consciousness. However it is possible that a rapid increase in blood glucose levels (after treating hypoglycaemia), may trigger a further episode of reactive hypoglycaemia in post bariatric patients. If you notice that this happens consistently, then you could try to reduce the initial amount of fast acting glucose administered. It has been suggested that a dose of 8-12 grams of carbohydrates may be suitable. As advised above, follow this up with a LGI carbohydrate and protein snack to help stabilise your blood glucose levels.
Food, symptom and activity diary
Glycaemic Index Food Table
The Glycaemic Index is a method of ranking the carbohydrate in foods according to how they affect blood glucose levels. Low GI foods are more slowly digested and absorbed by the body resulting in a more gradual and smaller rise in blood glucose levels (and therefore insulin levels).
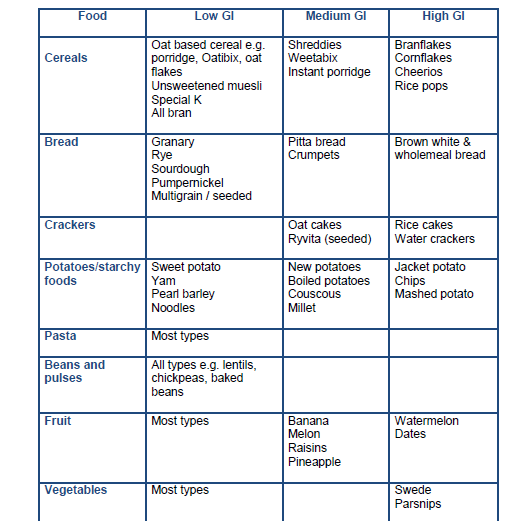
Resources:
- https://www.glycemicindex.com/
- British Dietetic Association: https://www.bda.uk.com/uploads/assets/faa872cd-98fb-4338-a92b0e37a8f39683/Glycaemic-Index-food-fact-sheet.pdf
High protein, low glycaemic index portion plate

- EAT FIRST: Protein
- EAT SECOND: Vegetables / salad
- EAT LAST: LGI carbohydrates
Reading food labels to work out the carbohydrate content in foods
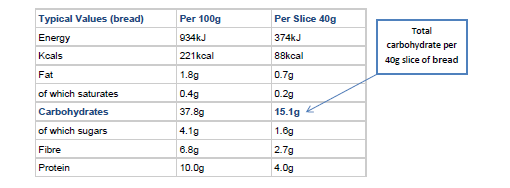
When reading the information on food labels the nutritional information is often given per 100 grams of food. When trying to work out the carbohydrate content, have a look to see if the information tells you how much carbohydrate is in a portion of the food you are likely to eat. The example above shows the carbohydrate content in a slice of bread. All carbohydrates are broken down in your body to glucose (sugars), so you should use the total amount of carbohydrates as opposed to that ‘of which sugars’.
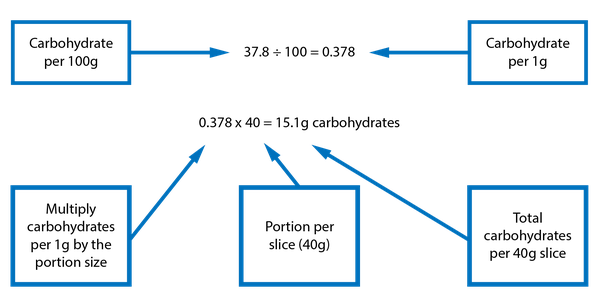
You can follow this calculation if the product does not have the nutritional information per serving.
The carbohydrate content of common foods
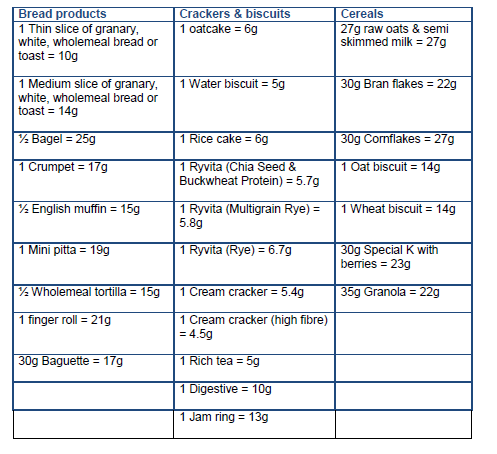
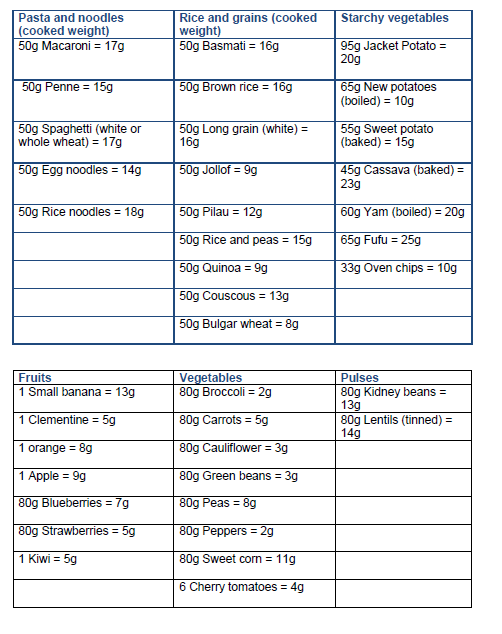
This list is to be used only as a guide. Please refer to the nutritional information on food labelling for accurate data.
Further resources:
The Carbs and Cals website have free resources to download:
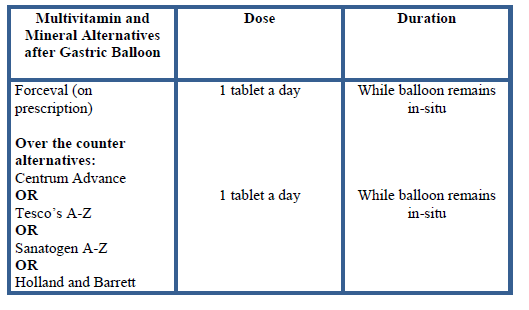
Vitamin and Mineral Supplements After Gastric Band and Balloon Insertion
After your band or balloon
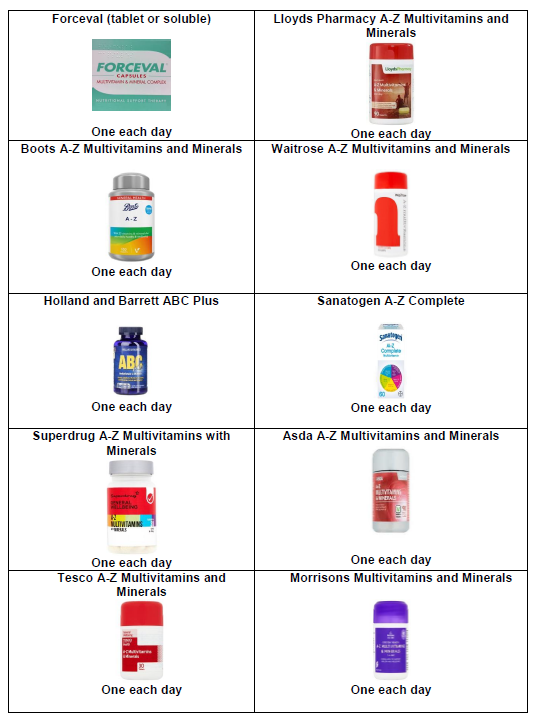
After your surgery you will need to take a complete multivitamin and mineral supplement every day for life (or for as long as you have a gastric band or balloon). Some multivitamins and minerals can be prescribed by your GP. Alternatively you can purchase some over the counter from pharmacies and supermarkets.
How much should I take?
Follow the instructions on the particular products packaging. However the dose for the majority of multivitamins and minerals is one capsule each day.
Why do I need to take a multivitamin and mineral every day?
After your surgery, you will begin to eat less than you did before. In the long term this can result in an inadequate intake of vitamins and minerals. Taking a daily multivitamin and mineral may help to supplement your intake and reduce the risk of deficiencies.
When should I start taking a multivitamin and mineral?
Start as soon as possible after your band insertion or balloon. If possible, take your supplement just before or after food as this may reduce side effects such as nausea.
Pregnancy
If you are planning a pregnancy you will need to ensure that your vitamin and mineral is suitable. During pregnancy you will need to avoid any supplements containing Vitamin A (in the form of retinol). Pregnancy specific multivitamins and minerals are suitable or any that contain Vitamin A in the form of beta carotene. Please speak to your Dietitian if you need advice.
Suitable vitamins and minerals
Contact information
Bariatric Dietitians: 0203 315 8161
Vitamin and Mineral Supplements after Gastric Bypass or Sleeve Gastrectomy
After your surgery
Multivitamin and Mineral supplements are mandatory for life after you have had a gastric bypass or sleeve gastrectomy.
Some multivitamins and minerals can be prescribed by your GP. Alternatively you can purchase some over the counter from pharmacies and supermarkets.
After surgery the quantity that you will be able to eat reduces and this combined with changes to your stomach and small intestine (that result in some mild malabsorption), will mean that you may not absorb sufficient vitamins and minerals. Daily vitamin and mineral supplements are essential to reduce the risk of any deficiencies and keep you well.
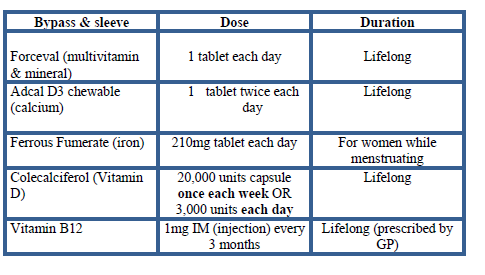
You will need the following:
A complete A-Z multivitamin and mineral formula – daily
Begin to take your multivitamin and mineral as soon as possible after surgery. You will be given a soluble formula (for 1 month) when you are discharged from hospital. After this your GP can prescribe you with tablets. Take your supplement with or after food to reduce the risk of side effects such as nausea.
Calcium and Vitamin D (combined) formula – 1200-1500mg/daily from food and supplements
Calcium is an essential mineral for your bone health, cell and muscle function, and is better absorbed with the presence of vitamin D.
Taking calcium and iron together can interfere with the others absorption, so take these supplements at separate times across the day, leaving at least a 2 hour gap between them.
An iron supplement – daily for women of menstrual age (or if you have anaemia)
Iron is essential for the formation of red blood cells that carry oxygen around the body. Iron deficiency can cause anaemia and symptoms include; fatigue, palpitations, pale skin, hair loss and a sore mouth.
Taking iron and calcium together can interfere with the others absorption, so take these supplements at separate times across the day, leaving at least a 2 hour gap between them.
A separate Vitamin D3 (in addition to calcium/Vitamin D combined supplement) – 20,000IU once each week (or 2,000-4,000IU daily)
Vitamin D helps regulate the amount of calcium and phosphate in the body. It helps to keep bones, teeth and muscles healthy. In adults Vitamin D deficiency can lead to bone pain caused by a condition called Osteomalacia in adults.
B12 (Hydroxycobalamin) 1mg intramuscular injection - every 3 months
Vitamin B12 is involved in helping the body make red blood cells and keeps the nervous system healthy. The changes to your stomach and small intestine after bariatric surgery can affect your absorption of B12.
Deficiency may result in fatigue, weakness, a sore, red tongue or mouth ulcers. More serious consequences of deficiency include; pins and needles, disturbed vision, depression, confusion, and problems with memory.
Take all of your vitamins and mineral every day but do not take them all together. Spread them evenly across the day to help your body absorb them.
Here is an example:
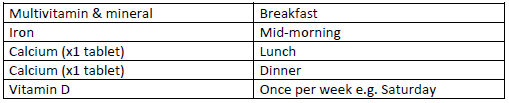
Paying for your prescriptions
If you are not eligible for free prescriptions, then you could consider a pre- payment certificate (PPC) to help with the costs of your supplements (and medications).
You can purchase this 3 monthly or yearly. For further information visit: https://www.nhsbsa.nhs.uk/help-nhs-prescription-costs/prescription-prepayment-certificates-ppcs
Below are lists of suitable multivitamins and minerals, some of which can be prescribed by your GP or alternatively purchased from pharmacies or online.
Suitable A-Z Vitamins and Minerals
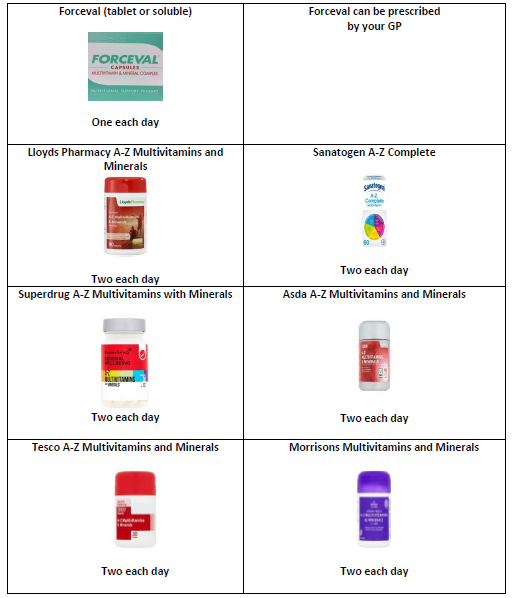
Suitable Calcium (with Vitamin D) supplements
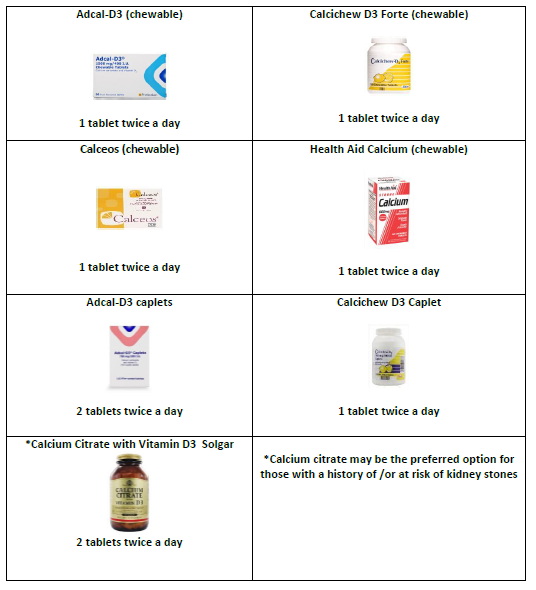
Suitable Iron supplements
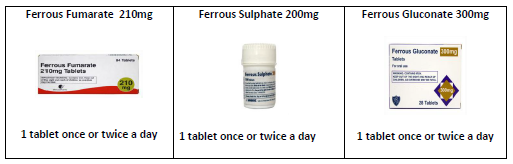
Suitable Vitamin D supplements
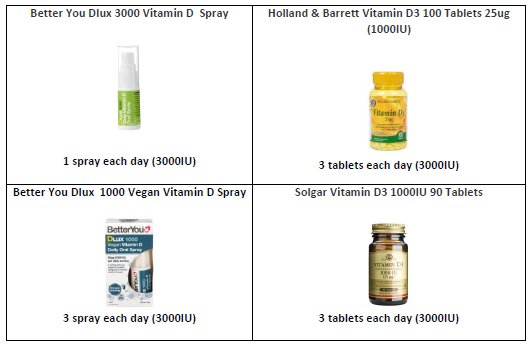
Baricol Complete
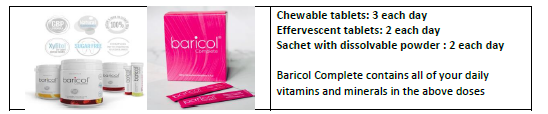
Thiamine
If you experience prolonged vomiting and/or poor dietary intake or excessive weight loss, then contact your dietitian or GP as you may require additional supplements of Thiamine and Vitamin B Co strong. These B Vitamins are not usually stored in the body so levels can become quickly depleted.
Symptoms of thiamine deficiency include; confusion, neuropathy (damage to the nerves), poor coordination (stumbling, falling), slurred speech and a rapid heart rate (tachycardia).
Bariatric Dietitians: 0203 315 8161
Pregnancy after Bariatric Surgery
Introduction
Bariatric surgery is an effective treatment option to reduce risks of weight-related co-morbidities and provide additional benefits in terms of fertility and pregnancy outcomes in women of childbearing age. However, it is recommended that you avoid pregnancy for at least 18 months after bariatric surgery as during this period you will be experiencing rapid weight loss. Therefore, you are most at risk of nutritional deficiencies which may cause both maternal and fetal complications during the pregnancy. In view of this, you are recommended to use contraception during the first 18 months post-surgery. Oral contraception may not provide sufficient protection after bariatric surgery (particularly in malabsorptive procedures such as gastric bypass) as lower absorption rates are suspected. Thus, it is recommended that you use an alternative method of contraception. You will need to discuss this with your GP or gynaecologist.
What happens when I find out I am pregnant after 18 months post-op?
- Speak to your GP about referral to an obstetrician at your local hospital. Your GP will need to inform the obstetrician of the importance of serial ultrasound examinations every 4 - 6 weeks to evaluate fetal growth from the 24th week of gestation, especially in women with poor weight gain as there is a possible increased risk of intrauterine growth restriction (IUGR) and small for gestational age (SGA) in post-bariatric surgery pregnancies.
- Contact the Bariatric Service immediately and inform them of your pregnancy so that follow-up appointments can be arranged with the bariatric dietitians.
- We will invite you to attend regular follow-up appointments with the bariatric dietitians at least every trimester. It is important for us to ensure you are eating the correct balance of nutrients and identify any nutritional deficiencies at an early stage so we can manage or treat them. You will be required to undergo regular nutritional blood tests at a minimum of every trimester taken either at the hospital or at your GP practice.
Nutrition during pregnancy
Management of nausea
Nausea and vomiting are common in pregnancy. Early management with dietary advice and/or clinically approved anti-emetics is recommended to avoid or treat complications. Dietary and behaviour changes to improve nutritional intake when nauseous include:
- Eating small and often meals
- Avoiding foods with strong odours
- Choosing cold food options
- Taking anti-emetics (if prescribed by your GP)
- Taking a short walk before meals
- Listing foods that particularly cause nausea and avoiding these for a period of time
Severe or prolonged nausea and vomiting may result in decreased nutritional intake, increased nutrient losses or poor nutrient absorption. This can increase the risk of thiamine deficiency. Therefore you may be required to take additional supplementation (Thiamine). If you are experiencing severe nausea and vomiting then please discuss with your dietitian and/or doctor.
Healthy eating
- It is important to eat a good variety of foods during pregnancy. These food groups include: protein rich foods, fruits and vegetables, dairy and dairy alternatives and starchy carbohydrates such as bread, rice, pasta, potatoes.
- Continue to prioritise protein containing foods such as chicken, red meat, fish, beans, lentils, tofu, soya, eggs, dairy and dairy alternatives.
- Aim to fill half of your plate with protein rich foods, and the remaining two quarters of the plate with vegetables or salad and carbohydrates. Remember your daily protein requirement: 70-100g per day.
- Choose healthy protein rich snacks in between meals such as a handful of nuts, hummus with carrot sticks, low-fat cheese and crackers, a protein bar, high protein yogurt, glass of skimmed/semi-skimmed milk, cooked chicken or ham slices, low-fat custard, rice pudding.
- Avoid snacks high in fat and sugar to prevent dumping syndrome symptoms and avoid excessive weight gain.
- Aim to drink at least 1.5-2L of fluids throughout the day (avoid sugary and fizzy drinks, and avoid alcohol).
- If you feel nauseous and cannot manage a meal, then try to have a protein shake or protein yoghurt as you may be able to tolerate this better.
- Continue to follow the golden rules; eating slowly, chewing thoroughly, separating eating and drinking, and stop eating when you feel full.
- Continue to use your side plate and small cutleries
Foods to avoid during pregnancy
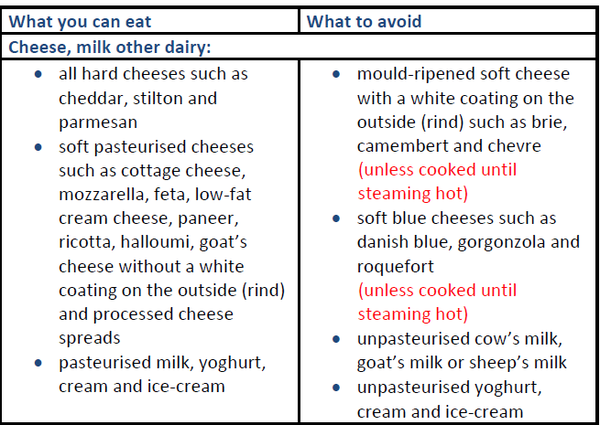
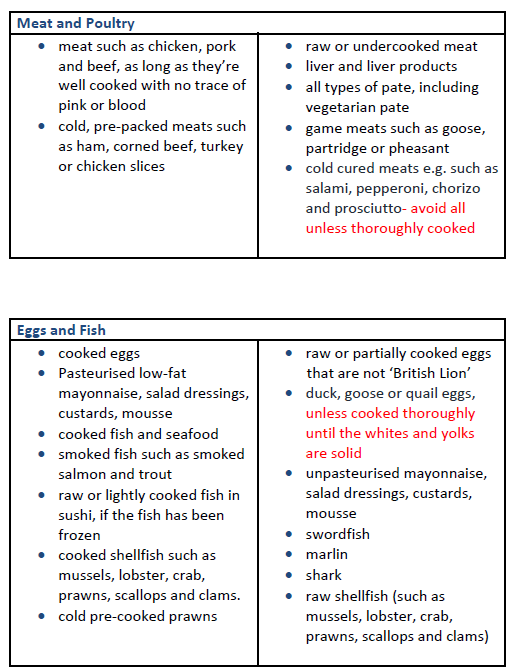
Fish and shellfish:
- You should not eat more than 2 portions of oily fish a week such as salmon, trout, mackerel, sardines or herring because they contain pollutants such as dioxins and polychlorinated biphenyls in them. If you eat too much of these, they can be harmful to your unborn baby.
- You should not eat more than 2 cooked tuna steaks (portion: about 140g cooked or 170g raw) or 4 medium-size cans of tuna (about 140g when drained) per week because it has more mercury in it than other fish. If you eat too much mercury, it can be harmful to your unborn baby.
- You should avoid raw shellfish because they can contain harmful bacteria, viruses or toxins in them. These can make you unwell and give you food poisoning.
Other foods and drinks
Caffeine
Limit caffeine intake no more than 200mg per day. There is:
- 100mg in a mug of instant coffee
- 140mg in a mug of filter coffee
- 75mg in a mug of tea (green tea can have the same amount of caffeine as regular tea)
- 40mg in a can of cola
- 80mg in a 250ml can of energy drink
- less than 25mg in a 50g bar of plain dark chocolate
- less than 10mg in a 50g bar of plain milk chocolate
Alcohol
If you're pregnant or planning to get pregnant, the safest approach is to not drink alcohol at all. Drinking alcohol in pregnancy can lead to long-term harm to your baby. Some studies also suggest an increased risk of alcohol dependency following bariatric surgery.
Vitamin and mineral supplementations during pregnancy following gastric bypass or sleeve gastrectomy
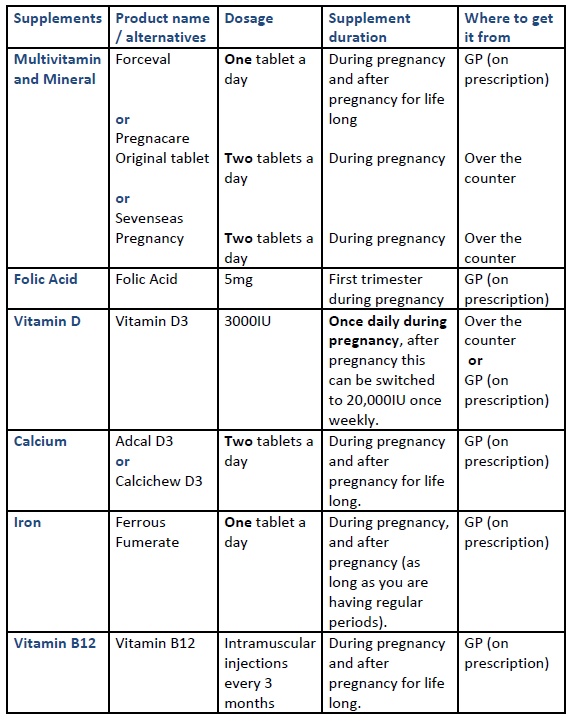
Vitamin and mineral supplementations required during pregnancy following gastric band
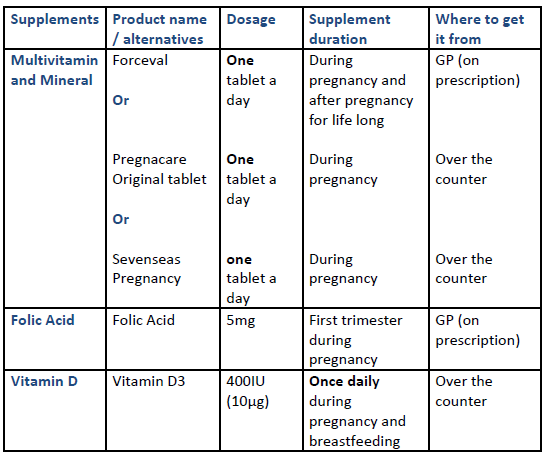
Considerations for patients with a gastric band
If you have a gastric band and become pregnant you will need to contact the specialist bariatric nurse to discuss whether your band will need be adjusted during your pregnancy. If the band is not adjusted accordingly it may cause an increase in the symptoms of nausea, vomiting, intolerance to foods and abdominal pain. Please note excessive vomiting may increase the risk of band slippage.
Expected weight gain during pregnancy
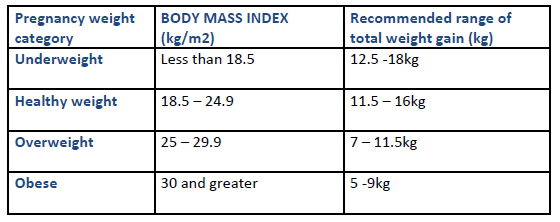
Breastfeeding
Your antenatal team will discuss feeding techniques, including breastfeeding during your pregnancy. Here are some points to consider:
- Breast milk is unique and meets a baby’s nutritional requirements. The World Health Organization (WHO) recommends exclusive breastfeeding until your baby is six months of age. From six months of age, babies require additional nutrition provided by solid foods (weaning), and breastfeeding alongside this is recommended. There are no known contraindications for mother’s breastfeeding after bariatric surgery.
- Breastfeeding normally uses around 500 calories a day once established. You do not usually need to eat extra calories for this (unless you have lost a lot of weight or are underweight). Continue to have regular protein rich meals and snacks, and foods rich in calcium such as dairy foods and dairy alternatives throughout the day, to ensure that you and your baby are receiving adequate nutrition.
- You are not required to take additional vitamins and minerals other than the usual post-operative recommendations summarised above. If you do not take your vitamins and minerals routinely, this may cause vitamin and mineral deficiencies that may affect the quality of your breast milk.
Useful links
Contact information
If you have any questions please contact the Bariatric Dietitians: 0203 315 8161

