Reactive Hypoglycaemia After Bariatric Surgery
What is Reactive Hypoglycaemia?
Reactive hypoglycaemia is the general term for hypoglycaemia (low blood glucose levels) after eating. It usually occurs a few hours after a meal, snack or drink (1-4 hours) and is a recognised complication after bariatric surgery.
What are the symptoms of reactive hypoglycaemia?
If these symptoms occur within 1-4 hours after eating, you may be experiencing reactive hypoglycaemia:
- Feeling sweaty
- Hungry
- Anxious
- Shaky
- Confusion
- Dizziness
- Difficulty coordinating movement S
- lurred speech
- Loss of consciousness
- Palpitations (rapid heart rate)
Why does reactive hypoglycaemia occur?
It is the result of the anatomical alterations to your gut and changes to gut hormones that occur after bariatric surgery and affect the way carbohydrates (sugars) are digested and absorbed. Reactive hypoglycaemia is closely linked to your diet and can often be managed with dietary changes.
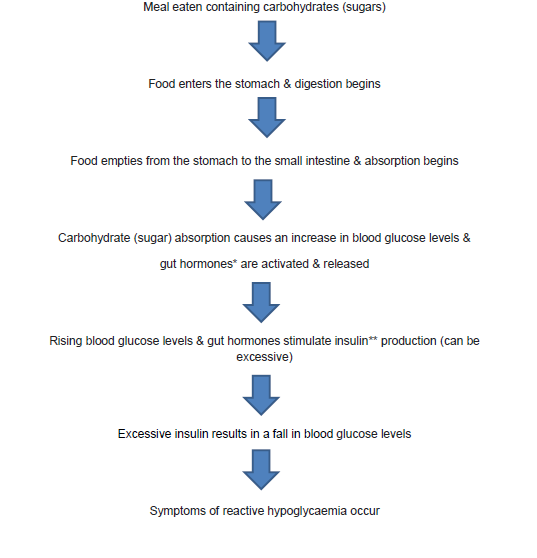
* Gut hormones: GLP 1 & Gastric inhibitory polypeptide
** Insulin is released in response to an increase in blood glucose levels. The role of insulin is to control blood glucose levels. It does this by signalling to the liver, muscle and fat cells to use glucose from the bloodstream for energy. If the body’s cells have enough energy then insulin signals to the liver to store the glucose as glycogen.
How is reactive hypoglycaemia diagnosed?
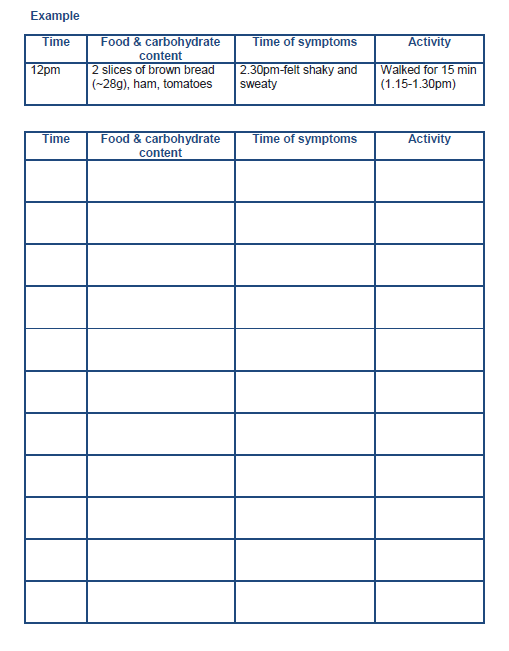
Keeping a food and symptom diary can be helpful to confirm (or not) whether any of the foods you eat are triggering symptoms. Record the type of food eaten, along with the amount and times of meals and symptoms using the diary in this booklet. This information can be shared with the Dietitian who can advise dietary changes to help improve your symptoms.
However, if the Dietitian is unable to help you manage your symptoms or your symptoms are severe, we will refer you to an Endocrinologist for further investigations and management.
Which Foods Contain Carbohydrate?
Carbohydrates can be divided into 2 groups; starchy (or complex) carbohydrates and free sugars.
Carbohydrates are found in; pasta, couscous, breakfast cereals, crackers, rice, fruit (fresh, tinned, dried), and starchy vegetables such as potatoes, yam and sweet potato. All of these are digested by your body to release glucose (sugar). Some processed foods that contain carbohydrates (free sugars) include; cakes and biscuits, sweets, chocolates, fruit juice and smoothies, jam, marmalade and honey.
Adapting your diet to manage reactive hypoglycaemia
The main principles:
- Eat small portions of food more regularly across the day
Ensure that meals and snacks are structured and spaced 3-4 hours apart so you do not have long gaps between eating. Eating 3 small meals and 2-3 snacks across the day can help to stabilise your blood glucose levels and avoid symptoms that may be caused by eating large portions of food (or carbohydrates).
- Try to limit your carbohydrates. Aim for 30g of carbohydrates at each main meal and 15g for snacks
Some studies have shown that limiting the amount of carbohydrates at mealtimes can help to avoid rapid rises in blood glucose levels after eating, excess insulin secretion and therefore avoid rapid drops in blood glucose levels that can result in the symptoms of reactive hypoglycaemia.
To begin with, it may be helpful to calculate the grams of carbohydrates you are currently having at mealtimes and if this amount causes symptoms then decrease it. For example, if you are having 2 thin slices of bread (around 20g carbohydrate) and this causes symptoms, then halve this to 1 slice (10g carbohydrate) to see if this prevents reactive hypoglycaemia. At the back of this booklet you will find a list of common foods with their average carbohydrate content, as well as other resources that you can use to calculate the carbohydrate content of food. Use the food and symptom diary to record the effects of any dietary changes.
- Choose Low Glycaemic Index carbohydrates
Carbohydrates are absorbed at different rates. Low Glycaemic Index (LGI) carbohydrates are digested and absorbed more slowly than High Glycaemic Index foods. Including a small amount of LGI carbohydrates at your meals may slow down the rise in blood glucose levels (after eating) and keep your blood glucose levels more stable afterwards. This may help to prevent (or reduce) symptoms of reactive hypoglycaemia. At the back of this booklet there is a list of some common LGI carbohydrates.
- Meet your protein recommendations (average of 70-100 grams/day)
Eat protein at all of your main meals and choose protein rich foods for snacks. Protein is important to preserve your muscle mass after surgery and it helps you to fill fuller for longer. Remember to prioritise protein, always eating this first during your meals or snacks.
- Eat more fibre
Fibre rich foods move more slowly from your stomach in to your small intestine. This can help to delay the increase in blood glucose levels after eating, decrease insulin secretion and therefore help to reduce the risk of reactive hypoglycaemia. Try to eat more fibre rich LGI foods such as oats, beans and pulses, granary bread, brown pasta, brown basmati rice and vegetables.
- Avoid eating and drinking together
Follow the ‘golden rules’ and separate eating and drinking. Avoid drinking less than 15 minutes before and wait 30 minutes after meals or snacks. Eating and drinking together can increase the rate at which food empties from your stomach into your small intestine that can cause a rapid rise in blood glucose levels and rapid secretion of insulin.
- Avoid sugary drinks
Avoid sugary drinks such as fruit juice, fizzy drinks, smoothies and milk shakes as these drinks are a source of carbohydrates (in liquid form) and are easily absorbed by the body. Sugary drinks can cause a rapid increase in blood glucose levels, as well as insulin and increase the risk of reactive hypoglycaemia. Suitable alternatives include; water, sugar free squash, tea, and coffee (with sweetener).
- Avoid alcohol
Alcohol can affect the way your liver produces and releases glucose so consumption may increase the risk of reactive hypoglycaemia. There is also some evidence that suggests an increased risk of alcohol dependency after bariatric surgery.
- Keep a food, symptom and activity diary
This can be useful and you can use it as a tool for reflection. Keeping a record of the times you eat, your symptoms and physical activity can help you identify triggers for your symptoms. In the long term if you are aware of your triggers, you can modify your diet to help you with managing your symptoms.
Treating severe symptoms of hypoglycaemia
If you experience severe symptoms of hypoglycaemia (confusion, difficulty coordinating, slurred speech) then you will need to administer some fast acting carbohydrate (in glucose form) to rapidly increase your blood glucose levels. The guidance suggests around 15 grams of glucose and some suitable options are:
- 3 Jelly babies
- 5 Glucotabs
- 5 Dextro energy tabs
- 4 Wine gums
- 175ml Lucozade energy (original)
- 60ml Lift Juice glucose shot
After 15-20 minutes of taking some fast acting carbohydrates your symptoms should begin to improve. You should then eat a small carbohydrate snack (if your next meal is not due). Opt for a LGI carbohydrate and some protein as this may help stabilise your blood glucose levels. A suitable option would be 1or 2 oat cakes (LGI) with some low fat cheese or a slice of cooked meat.
The purpose of treating hypoglycaemia is to rapidly increase your blood glucose level and reduce the risk of more severe symptoms of hypoglycaemia such as loss of consciousness. However it is possible that a rapid increase in blood glucose levels (after treating hypoglycaemia), may trigger a further episode of reactive hypoglycaemia in post bariatric patients. If you notice that this happens consistently, then you could try to reduce the initial amount of fast acting glucose administered. It has been suggested that a dose of 8-12 grams of carbohydrates may be suitable. As advised above, follow this up with a LGI carbohydrate and protein snack to help stabilise your blood glucose levels.
Food, symptom and activity diary
Glycaemic Index Food Table
The Glycaemic Index is a method of ranking the carbohydrate in foods according to how they affect blood glucose levels. Low GI foods are more slowly digested and absorbed by the body resulting in a more gradual and smaller rise in blood glucose levels (and therefore insulin levels).
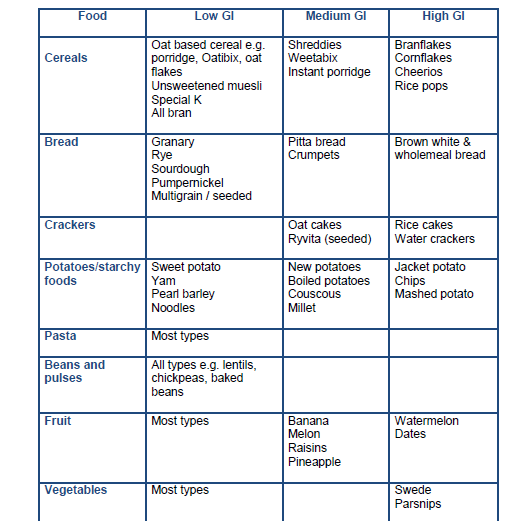
Resources:
- https://www.glycemicindex.com/
- British Dietetic Association: https://www.bda.uk.com/uploads/assets/faa872cd-98fb-4338-a92b0e37a8f39683/Glycaemic-Index-food-fact-sheet.pdf
High protein, low glycaemic index portion plate

- EAT FIRST: Protein
- EAT SECOND: Vegetables / salad
- EAT LAST: LGI carbohydrates
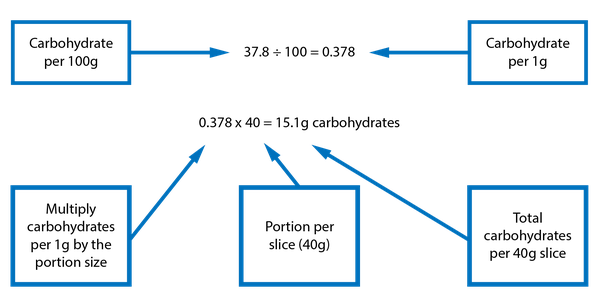
Reading food labels to work out the carbohydrate content in foods
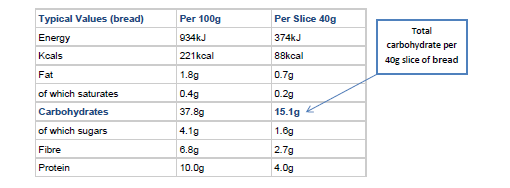
When reading the information on food labels the nutritional information is often given per 100 grams of food. When trying to work out the carbohydrate content, have a look to see if the information tells you how much carbohydrate is in a portion of the food you are likely to eat. The example above shows the carbohydrate content in a slice of bread. All carbohydrates are broken down in your body to glucose (sugars), so you should use the total amount of carbohydrates as opposed to that ‘of which sugars’.
You can follow this calculation if the product does not have the nutritional information per serving.
The carbohydrate content of common foods
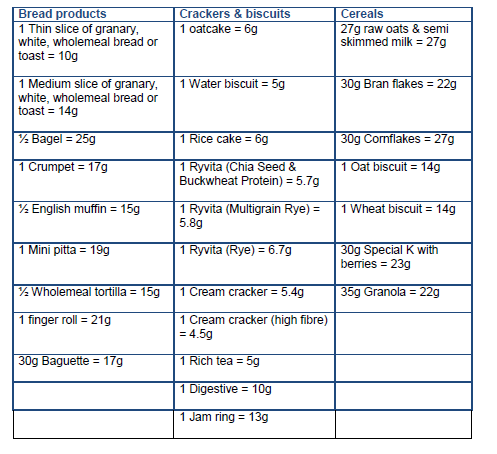
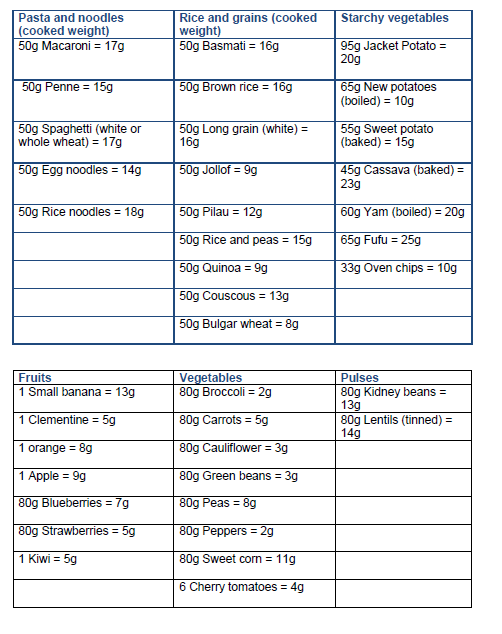
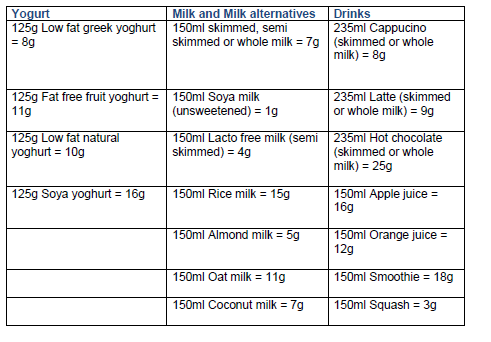
This list is to be used only as a guide. Please refer to the nutritional information on food labelling for accurate data.
Further resources:
The Carbs and Cals website have free resources to download:

