Dietary Guidance after Intra-gastric Balloon Insertion
Introduction
The intra-gastric balloon is a soft silicone balloon that is placed inside the stomach and filled with saline (sterile water) and some blue dye. By taking up space within your stomach, the balloon helps you feel full from a smaller amount of food. Together with a balanced diet and increased physical activity levels an intra-gastric balloon can help you lose weight.
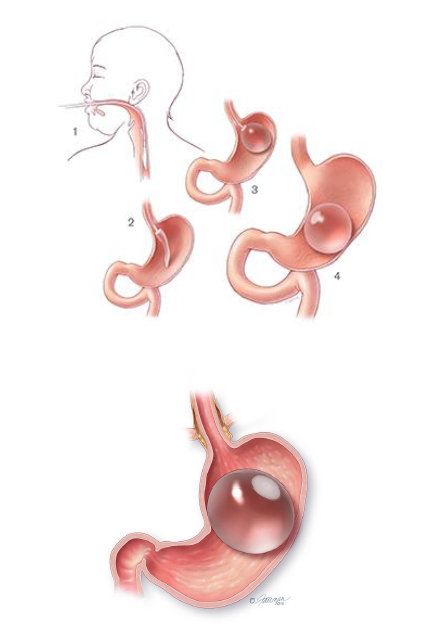
What happens during intra-gastric balloon insertion?
The balloon will be inserted through a tube down your throat either under light sedation, or under general anaesthetic. The tube will not interfere with your breathing at any time as it passes down your oesophagus not into your wind pipe.
Once in your stomach the balloon is inflated with saline and some blue dye. The volume of saline inserted varies from 500–700mls. Once inflated, the balloon is too large to pass into the bowel and it will float freely inside the stomach. The procedure generally takes 20–30 minutes.
How long does the balloon stay in place?
The balloon can remain inside for 6 to 12 months. Longer periods of use are not recommended as over the time the acid content of the stomach will weaken the balloon material and cause the balloon to deflate.
How much weight will I lose with the balloon?
The amount of weight you lose can vary but on average people lose up to 20kg through balloon, diet and physical activity.
Do I need to follow a specific diet prior to balloon insertion?
Your stomach must be completely empty prior to balloon insertion.
Therefore, you must stop eating for at least 6 hours, and drink any liquids for 4 hours, before the procedure.
If you are required to take any specific medication at a specific time then you are advised to consult to your GP or bariatric team for further advice.
Do I need to follow a specific diet prior to balloon removal?
For intragastric balloon removal, it is necessary to follow a clear liquid only diet for 3 days prior to your scheduled procedure date.
During this time you should consume a clear liquid diet consisting of only the following:
- Water
- Black tea or black coffee (no sugar)
- Broth
- Vegetable juice (no pulp)
- Squash (no added sugar)
Post-operative Diet
This information will guide you through the post- operative stages step-by- step after gastric band insertion.
The texture progression phases from fluids to solids are important to reduce the risk of unpleasant side effects such as nausea, vomiting, pain and discomfort. Therefore it is important not to skip any of the stages.
You will need to follow a modified texture diet for 2 weeks, before returning to a regular texture diet. The diet is separated into 4 separate stages:
- Liquids
- Puree
- Soft
- Regular
Stage 1 – only smooth liquids for 1 week (day 0-7)
You can start to take sips of fluids as soon as you feel able to. To get the most success from the balloon you must wait about 20–30 minutes after eating before having a drink—this will also help to wash any food debris that may have become stuck to the balloon. Remember to sit upright during and after meals. Drink small quantities throughout the day—do not allow yourself to become too thirsty as you will not be able to drink large quantities at a time. Start with sips (little and often), and if you feel comfortable then gradually increase the amount.
- Avoid fizzy/carbonated drinks and alcohol
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
- All liquids should be completely smooth with no bits or lumps (e.g. can be sucked through a straw).
- Avoid big gulps as this may cause discomfort, nausea, sickness and regurgitation.
Which liquids are suitable?
- Skimmed or semi-skimmed milk or lacto-free or soya milk (try adding dried skimmed milk powder or protein powder)
- High protein shakes
- SlimFast or alternative meal replacement shake
- Low-fat natural or plain yoghurt drinks
- Complan soup
- Meritene soup
- Protein Water
Other fluids you can have:
- Still water
- Marmite®, Bovril®, consommé, bouillon
- Clear soups
- Herbal or fruit teas
- Tea and coffee (use sweeteners, not sugar)
- No added sugar/sugar free squash
- Sugar free jelly
- Diluted vegetable juice (no bits)
Sample meal plan
- Breakfast: High protein shake
- Lunch: SlimFast shake or Meritene/Complan soup (1 sachet)
- Evening meal: High protein shake or Meritene/Complan Soup
- Snacks in between meals: if you feel hungry in between meals you can consume 200ml of skimmed/semi-skimmed/lacto-free/soya milk 8
Stage 2 – only puree foods for 4 days (day 8-11)
All food during this stage should be pureed and completely smooth with no bits or lumps.
Puree foods are smooth and can pass through your stomach easily. You must use a blender, liquidiser or a food processor to puree your food to the correct consistency. Aim for a smooth consistency like ‘yoghurt’.
Try to include foods that are high in protein in your meals to keep you fuller for longer.
How much and when?
Eat 5-6 small meals throughout the day during this stage. Start with 1-2 tablespoons at your meals and snacks, and if you feel comfortable gradually increase the amount.
As you progress through the puree stage, you may find that your portions gradually increase. However, remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
- Avoid fizzy/carbonated/sugary drinks and alcohol.
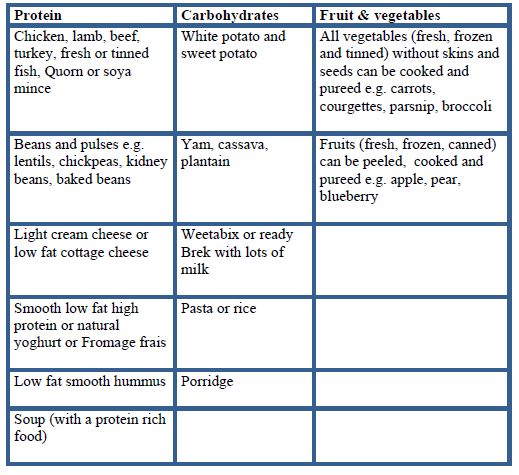
Which foods are suitable?
All of the foods in the table below are suitable, and will need to be pureed.
Sample meal plan
Breakfast:
Weetabix, Oatibix OR Ready Brek with plenty of skimmed/semi-skimmed/lacto-free/soya milk OR high protein yogurt pot or pouch
Lunch and Dinner ideas:
- Puree chicken with potato and vegetables
- Puree spaghetti bolognaise and vegetables
- Puree lentil or vegetable or chicken soup
- Puree tinned fish (tuna, sardines, and mackerel) with potato and vegetables
- Puree baked beans/tinned chickpeas.
Snacks:
Low-fat yogurt (with no bits), low-fat humous, low-fat custard with pureed fruit, smoothie (with no bits), home-made milkshake (with no bits, healthy recipe)
Stage 3 – soft, fork-mashable foods for 3 days (day 12-14)
Soft foods are foods that have a soft consistency, are well cooked that can easily be mashed with a fork. You do not need to use a blender during the soft stage.
Foods to avoid:
Avoid any foods that are hard or contain skins, seeds and pips as these will be difficult to mash into a soft consistency
- Sweet corn, peas, celery, fresh tomato, potato skin, nuts, seeds, hard cheese
- Dry, crumbly foods e.g. biscuits, crackers
- Food that has a mixed consistency e.g. minestrone soup, cereal flakes with milk
- Avoid fizzy/carbonated/sugary drinks and alcohol
How much and when?
Eat 3 meals a day and if you feel hungry between your meals, then have a snack. Use a small plate for your main meals, ¾ of your plate should include a protein and vegetables, and the remaining ¼ of your plate should include carbohydrates. Remember to stop eating at the first signs of fullness or if you feel uncomfortable. If you eat too much then you may experience pain, nausea and vomiting.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated.
Sample meal plan
Breakfast ideas:
- Porridge, Oatibix or Weetabix with skimmed milk
- Mashed baked beans
- Soft cooked eggs e.g. scrambled, poached, omelette
Lunch and Dinner ideas:
- Tinned or soft flaky fish with mashed potato and vegetables
- Shepherd’s pie or cottage pie with mashed vegetables
- Minced chicken/beef/lamb/turkey with couscous/mashed potato and vegetables
- Minced quorn or soya mince with pasta and vegetable
- Omelette with low fat grated cheese with mashed, peeled, seedless tomato
- Cauliflower cheese
- Risotto with soft mashed vegetables
- Chicken or meat casserole
- Thick soups e.g. lentil, ham, leek and potato
- Chicken/fish/beef/lamb/vegetable stews
Snack ideas:
200ml glass of skimmed milk (add 1-2 tsp of skimmed milk powder) or high protein shake or high protein yoghurt or low fat custard or low fat yoghurt
Stage 4 – Regular foods from day 15 and onwards
From day 15 and onwards you can gradually introduce regular texture foods and increase the variety of foods in your diet.
Continue to eat 3 regular meals each day and try not to leave more than 3-4 hours between meals.

- EAT FIRST -Protein (meat, fish, poultry, eggs, beans, pulses)
- EAT SECOND- Vegetables and salad
- EAT LAST - Carbohydrates (bread, rice, potato, pasta, grains)
Eating Guidance
- You should not graze (eat small amounts of food constantly through the day) or go for a long-period of time without eating.
- Aim to have 1.5-2 litres of fluids each day to stay hydrated. Avoid having large quantities at atime.
- Limit alcohol intake, you are allowed to have 1 or 2 glasses of alcoholic beverage on social occasions only.
- Avoid high fat, high calorie foods, snacks and sugary drinks as these will not assist with weight loss.
- Aim to eat slowly, chew thoroughly, separate eating and drinking.
- Aim to have a drink 30minutes after you have finished eating to ‘rinse’ the balloon
- Use a side plate to help guide your portions and follow the plate model below.
- If you are hungry in-between meals then choose a nutritious snack such as a piece of fruit, high protein yoghurt, handful of mixed nuts or a glass of skimmed/semi skimmed/soya/lacto-free milk.
Possible problem foods
There may be foods after an intra-gastric balloon insertion that some people find difficult to tolerate and feel like they get ‘stuck’ or may make you sick. These include; firm or dry red and white meat, bread, rice and pasta.
Possible Side Effects:
There can be some side effects to having the balloon inserted; the most common ones are listed below:
Nausea and vomiting
Nausea and vomiting are very common after the procedure. You will be given anti-sickness medication to help control this. It is common however, to have these symptoms for a couple of weeks after the procedure as your stomach adjusts to the balloon being in place.
To help with nausea make sure you are chewing your food thoroughly, separate eating and drinking and consume small portions.
Try moving around even if you don’t feel like it, as it will help the food to move from the stomach into the gut.
If you are struggling to keep any fluids down after the first four days or if you are concerned, please contact the hospital team.
Reduced stool volumes or reduced frequency of bowel movements
This is common and normally relates to the smaller amount of food being eaten. Normal bowel movements can be anything from 3 times per day to 3 times per week.
If your stool is hard to pass, make sure you are drinking enough water throughout the day (most people need about 2 litres per day). You should also aim to include fibre foods in your diet such as fruit, vegetables and wholegrain cereals/breads. These foods will help to relieve constipation and also tend to be low in calories and filling.
Heartburn and acid reflux
Heartburn and acid reflux are common after balloon insertion and medication will be prescribed to help control this. Some foods, such as caffeine, alcohol, spicy and fatty foods, can make reflux worse, if taken in large quantities.
Small amounts of low-fat milk and dairy products can help with acid reflux as can staying upright after meals and stopping eating at least 2 hours before going to bed.
You will be given some medication while you are in hospital (usually lansoprazole) to reduce stomach acid and prevent stomach ulcers forming. You will be given a small supply of this medication to take home with you when you are discharged. It is essential that you continue to take this medication for the whole time you have the balloon in place. Please make sure to contact your GP for a repeat prescription once the hospital supply has finished.
Odour associated with belching/burping
Bad –smelling belching or burping can be a problem and is likely related to food getting stuck in and around the mucous that coats the balloon. To avoid this, ensure you have a drink 30 minutes after eating, chew your food well and try to move around a lot as this can help stop the food from getting stuck.
Bloating
This is common and is caused by the balloon sitting in the stomach. Unfortunately there is little that can be done for this other than to have the balloon removed. Try to remember that although bloating can be uncomfortable the balloon is only temporary and is there to help you reduce your weight. If you are unable to tolerate the discomfort from bloating the balloon will need to be removed.
What happens if the balloon deflates spontaneously?
If the balloon deflates before a scheduled removal you should notice blue dye in your urine or stools. Contact the team and come to our A&E Department immediately so we can remove the balloon.
Vitamins and minerals
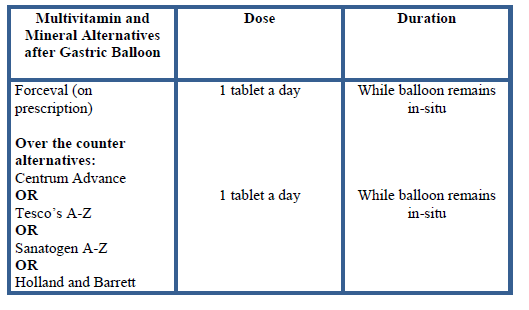
Due to the reduced portion sizes and overall food intake, you will not get adequate vitamins and minerals from the diet. Therefore you will need to start taking an additional vitamin and mineral supplementation once daily. As soon as you are able to start having liquids, you can begin taking your multivitamin and mineral supplement.