Pregnancy after Bariatric Surgery
Introduction
Bariatric surgery is an effective treatment option to reduce risks of weight-related co-morbidities and provide additional benefits in terms of fertility and pregnancy outcomes in women of childbearing age. However, it is recommended that you avoid pregnancy for at least 18 months after bariatric surgery as during this period you will be experiencing rapid weight loss. Therefore, you are most at risk of nutritional deficiencies which may cause both maternal and fetal complications during the pregnancy. In view of this, you are recommended to use contraception during the first 18 months post-surgery. Oral contraception may not provide sufficient protection after bariatric surgery (particularly in malabsorptive procedures such as gastric bypass) as lower absorption rates are suspected. Thus, it is recommended that you use an alternative method of contraception. You will need to discuss this with your GP or gynaecologist.
What happens when I find out I am pregnant after 18 months post-op?
- Speak to your GP about referral to an obstetrician at your local hospital. Your GP will need to inform the obstetrician of the importance of serial ultrasound examinations every 4 - 6 weeks to evaluate fetal growth from the 24th week of gestation, especially in women with poor weight gain as there is a possible increased risk of intrauterine growth restriction (IUGR) and small for gestational age (SGA) in post-bariatric surgery pregnancies.
- Contact the Bariatric Service immediately and inform them of your pregnancy so that follow-up appointments can be arranged with the bariatric dietitians.
- We will invite you to attend regular follow-up appointments with the bariatric dietitians at least every trimester. It is important for us to ensure you are eating the correct balance of nutrients and identify any nutritional deficiencies at an early stage so we can manage or treat them. You will be required to undergo regular nutritional blood tests at a minimum of every trimester taken either at the hospital or at your GP practice.
Nutrition during pregnancy
Management of nausea
Nausea and vomiting are common in pregnancy. Early management with dietary advice and/or clinically approved anti-emetics is recommended to avoid or treat complications. Dietary and behaviour changes to improve nutritional intake when nauseous include:
- Eating small and often meals
- Avoiding foods with strong odours
- Choosing cold food options
- Taking anti-emetics (if prescribed by your GP)
- Taking a short walk before meals
- Listing foods that particularly cause nausea and avoiding these for a period of time
Severe or prolonged nausea and vomiting may result in decreased nutritional intake, increased nutrient losses or poor nutrient absorption. This can increase the risk of thiamine deficiency. Therefore you may be required to take additional supplementation (Thiamine). If you are experiencing severe nausea and vomiting then please discuss with your dietitian and/or doctor.
Healthy eating
- It is important to eat a good variety of foods during pregnancy. These food groups include: protein rich foods, fruits and vegetables, dairy and dairy alternatives and starchy carbohydrates such as bread, rice, pasta, potatoes.
- Continue to prioritise protein containing foods such as chicken, red meat, fish, beans, lentils, tofu, soya, eggs, dairy and dairy alternatives.
- Aim to fill half of your plate with protein rich foods, and the remaining two quarters of the plate with vegetables or salad and carbohydrates. Remember your daily protein requirement: 70-100g per day.
- Choose healthy protein rich snacks in between meals such as a handful of nuts, hummus with carrot sticks, low-fat cheese and crackers, a protein bar, high protein yogurt, glass of skimmed/semi-skimmed milk, cooked chicken or ham slices, low-fat custard, rice pudding.
- Avoid snacks high in fat and sugar to prevent dumping syndrome symptoms and avoid excessive weight gain.
- Aim to drink at least 1.5-2L of fluids throughout the day (avoid sugary and fizzy drinks, and avoid alcohol).
- If you feel nauseous and cannot manage a meal, then try to have a protein shake or protein yoghurt as you may be able to tolerate this better.
- Continue to follow the golden rules; eating slowly, chewing thoroughly, separating eating and drinking, and stop eating when you feel full.
- Continue to use your side plate and small cutleries
Foods to avoid during pregnancy
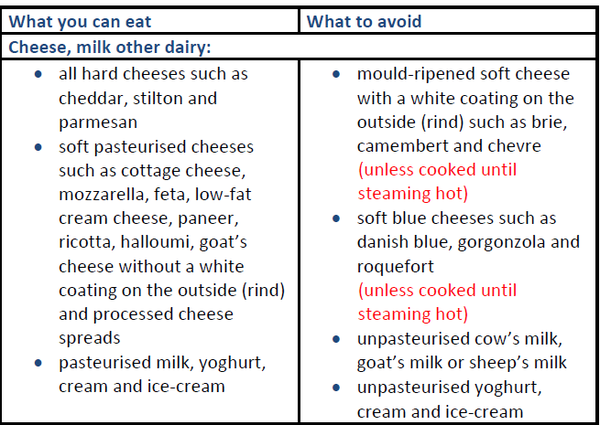
Fish and shellfish:
- You should not eat more than 2 portions of oily fish a week such as salmon, trout, mackerel, sardines or herring because they contain pollutants such as dioxins and polychlorinated biphenyls in them. If you eat too much of these, they can be harmful to your unborn baby.
- You should not eat more than 2 cooked tuna steaks (portion: about 140g cooked or 170g raw) or 4 medium-size cans of tuna (about 140g when drained) per week because it has more mercury in it than other fish. If you eat too much mercury, it can be harmful to your unborn baby.
- You should avoid raw shellfish because they can contain harmful bacteria, viruses or toxins in them. These can make you unwell and give you food poisoning.
Other foods and drinks
Caffeine
Limit caffeine intake no more than 200mg per day. There is:
- 100mg in a mug of instant coffee
- 140mg in a mug of filter coffee
- 75mg in a mug of tea (green tea can have the same amount of caffeine as regular tea)
- 40mg in a can of cola
- 80mg in a 250ml can of energy drink
- less than 25mg in a 50g bar of plain dark chocolate
- less than 10mg in a 50g bar of plain milk chocolate
Alcohol
If you're pregnant or planning to get pregnant, the safest approach is to not drink alcohol at all. Drinking alcohol in pregnancy can lead to long-term harm to your baby. Some studies also suggest an increased risk of alcohol dependency following bariatric surgery.
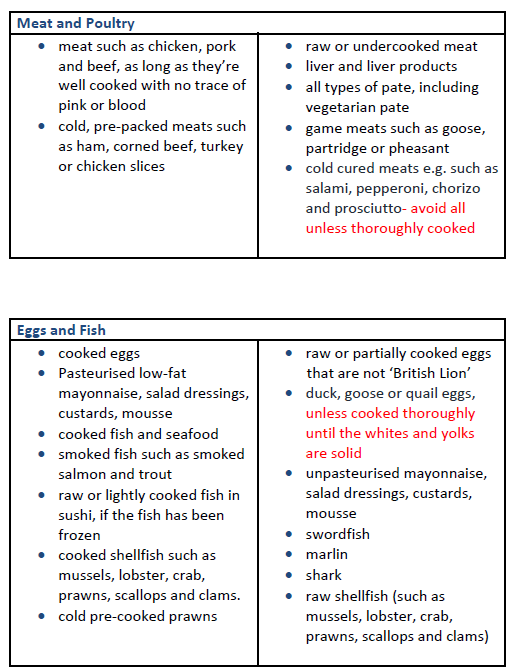
Vitamin and mineral supplementations during pregnancy following gastric bypass or sleeve gastrectomy
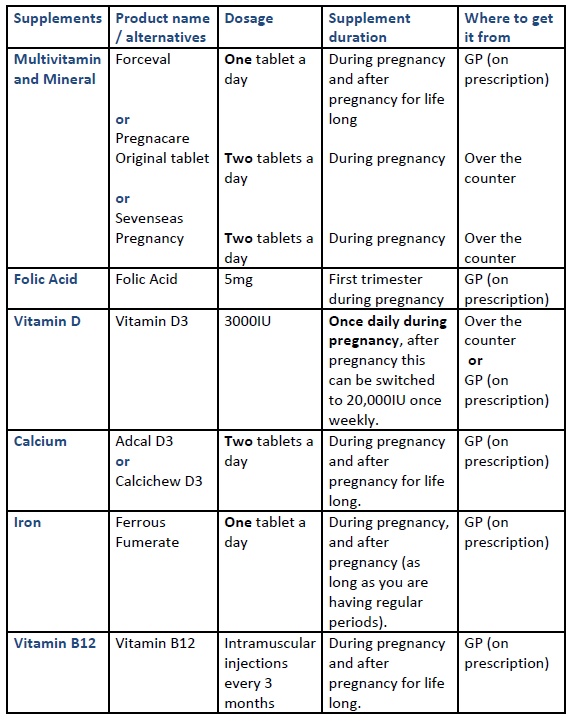
Vitamin and mineral supplementations required during pregnancy following gastric band
Considerations for patients with a gastric band
If you have a gastric band and become pregnant you will need to contact the specialist bariatric nurse to discuss whether your band will need be adjusted during your pregnancy. If the band is not adjusted accordingly it may cause an increase in the symptoms of nausea, vomiting, intolerance to foods and abdominal pain. Please note excessive vomiting may increase the risk of band slippage.
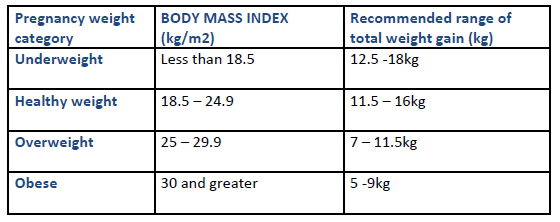
Expected weight gain during pregnancy
Breastfeeding
Your antenatal team will discuss feeding techniques, including breastfeeding during your pregnancy. Here are some points to consider:
- Breast milk is unique and meets a baby’s nutritional requirements. The World Health Organization (WHO) recommends exclusive breastfeeding until your baby is six months of age. From six months of age, babies require additional nutrition provided by solid foods (weaning), and breastfeeding alongside this is recommended. There are no known contraindications for mother’s breastfeeding after bariatric surgery.
- Breastfeeding normally uses around 500 calories a day once established. You do not usually need to eat extra calories for this (unless you have lost a lot of weight or are underweight). Continue to have regular protein rich meals and snacks, and foods rich in calcium such as dairy foods and dairy alternatives throughout the day, to ensure that you and your baby are receiving adequate nutrition.
- You are not required to take additional vitamins and minerals other than the usual post-operative recommendations summarised above. If you do not take your vitamins and minerals routinely, this may cause vitamin and mineral deficiencies that may affect the quality of your breast milk.
Useful links
Contact information
If you have any questions please contact the Bariatric Dietitians: 0203 315 8161

