Blood clots—DVT and PE information for inpatients
This information has been produced by the hospital Thrombosis and Thromboprophylaxis Group to help explain how a blood clot can develop and become a deep vein thrombosis (DVT) or a pulmonary embolism (PE). It will also discuss the signs and symptoms of blood clots. We hope it answers some of the questions you may have.
DVT (deep vein thrombosis)
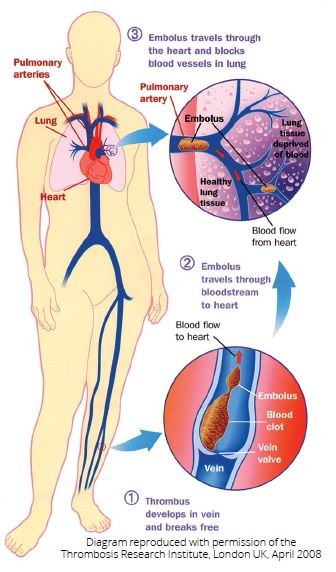
Deep vein thrombosis (DVT) is a common medical condition which occurs when a thrombus (blood clot) forms in a deep vein, usually in the leg or the pelvis. DVT can block off or reduce the flow of blood in the vein.
DVT in the leg or the pelvis can cause pain and swelling in the leg and may result in lifelong disability with painful leg swelling, varicose veins and leg ulcers.
PE (pulmonary embolism)
Sometimes the DVT (blood clot) in the leg breaks off and travels to the arteries of the lung where it will cause a pulmonary embolism (PE). PE may cause breathing difficulties and chest pain, and may be fatal.
VTE (venous thromboembolism)
DVT and PE are known under the collective term of venous thromboembolism (VTE).
How common are blood clots in hospital?
We often hear about the risks of DVT on long distance flights, but DVT is more likely to occur in patients who have stayed in hospital:
- In England each year, 25 times more people die from preventable VTE contracted in hospital than from MRSA infection
- 1 in 3 people having an operation in hospital can develop VTE if no preventative measures are taken
- 7 out of 10 deaths from VTE in hospital occur in medical patients (those who have not had an operation)
Are you at risk of blood clots in hospital?
There are several factors that may increase the chances of developing VTE in hospital. If you have more than one of these factors, you may be considered to be at increased risk:
- If you are older than 60 years of age—the risk of VTE is higher the older you are (but young people can also get blood clots)
- If you have previously had DVT or PE or a close member of your family (parents or brothers and sisters) has had DVT or PE
- If you have certain illnesses such as active cancer, heart failure, lung disease or infections (eg pneumonia)
- If you are immobile (especially if you are confined to your bed in hospital)
- If you are obese
- If you are pregnant
- If you are having major surgery, including orthopaedic surgery
- If you are taking a certain contraceptive pill or hormone replacement therapy tablets—your doctor may advise you to stop taking it before your surgery
What can you do to reduce the risk of developing blood clots before coming into hospital for a planned operation/procedure?
- Keep mobile—move around as much as possible in the weeks leading up to hospital admission.
- Take care on journeys—if you can, avoid long, uninterrupted journeys of more than four hours (for any long journeys, keep your legs and feet active).
- Medications—talk to your doctor if you are taking the contraceptive pill, hormone replacement therapy tablets, anticoagulants (known as ‘blood-thinning drugs’ for the treatment or prevention of blood clots) or antiplatelet therapy for appropriate management.
Will your risk of blood clots be assessed in hospital?
A doctor or a nurse will assess your risk of VTE when you are admitted to hospital. Your risk will be reassessed during your hospital admission to ensure any new risk factors are identified.
Ask your doctor or nurse, what is my risk of blood clots?
What will be done to reduce your risk of developing blood clots in hospital?
If you are considered to be at increased risk of developing DVT or PE in hospital, preventative measures may be taken:
- Anticoagulants—you may be given medication to thin your blood and prevent blood clots, known as anticoagulants. Like all medications, there is a risk of experiencing side effects— the main side effect is a slightly increased risk of bleeding. The blood thinner most often used is a type of heparin, which is given by injection. Please be aware that some blood thinners are derived from animal (pig) origin. Please discuss this with your doctor or nurse if this is a concern to you.
- Compression stockings—to help the blood flow in your veins.
- Calf pumps—may be put on your legs in the operating theatre during your operation to help the blood flow in your veins.
Ask your doctor or nurse, what is being done to reduce my risk of blood clots?
What happens when you are discharged from hospital?
Some patients may need to continue anticoagulation medication at home— your doctor, nurse or pharmacist will discuss this with you. You will be told how long to continue taking the anticoagulant medication, and what to do and who to contact should you experience any side-effects.
Please speak to your doctor, nurse or pharmacist if you have any concerns.
If you are having injections, you, a member of your family or a carer will be shown how to give the injections. If you, a member of your family or a carer are unable to give the injections, then your nurse will arrange for someone else to give you the injections when you are at home.
 |
You will be provided with a sharps bin to dispose of any sharps (needles) safely. |
 |
Compression stockings, if required and appropriate, should be worn while you are in hospital and until you return to your usual level of mobility. |
How will you know if you have DVT or PE?
The symptoms of DVT in the leg include:
- Swelling
- Pain
- Warm skin
- Tenderness
- Redness (particularly at the back of your leg below the knee)
DVT usually (although not always) affects one leg. In some cases, there may be no signs or symptoms of DVT at all in the leg.
The symptoms of PE include:
- Shortness of breath
- Pain in your chest that is worse when you breath in
- Collapse (in severe cases)
Both DVT and PE are serious conditions that require urgent investigation and treatment.
If you suspect you may have DVT or PE, you should seek medical advice immediately either from your GP or nearest A&E (Emergency Department).
Do the preventative measures to reduce the risk of developing blood clots have any possible side effects?
Medication
- The anticoagulant medication increases the time it takes your blood to clot and can make you bleed and bruise more easily—your risk of bleeding will be assessed with your risk of VTE
Tell your doctor or nurse if you experience any of the following side effects:
- Long or excessive bleeding
- Unexplained bruising
- Unusual headaches
Compression stockings
- If you are having an operation or you are unable to take anticoagulant medication, then you may be offered compression stockings
- You will be measured and fitted with compression stockings according to your leg measurements
- You will be shown how to wear them—this may help reduce your risk of developing VTE
- Tell your doctor or nurse if you have any marking, blistering, pain, discomfort or discolouration of skin on your feet, heels or legs
- You should remove your compression stockings every day so you can wash your legs and check your skin for any changes
Alternatives to compression stockings
Your doctor or nurse may ask you to wear a special inflatable sleeve or cuff around your legs while you are in bed—this will inflate automatically and provide pressure at regular intervals, increasing blood flow in your legs.
To be effective, VTE prevention measures must be used and administered correctly.
What can you do to help reduce your risk of developing blood clots in hospital and at home?
The risk of developing DVT or PE can continue after you have gone home. It is important to:
- Keep mobile (move around)
- Exercise
- Keep well-hydrated by drinking plenty of water
How can you help reduce your risk of blood clots?
Here is a simple exercise you can do, even when you are lying in bed, to help your blood move around your body:
 |
|
Who can you contact for more information?
If you would like any more information or have any questions, please ask a doctor, nurse or pharmacist. Further information can be found from NHS.uk or Thrombosis UK.

