Blood clots—Atrial Fibrillation (AF)
This leaflet has been produced by the hospital Thrombosis and Thromboprophylaxis Group to help explain atrial fibrillation (AF) including anticoagulation treatment and management.
Atrial Fibrillation (AF)
Atrial fibrillation (AF) is a heart condition that causes an irregular (out of rhythm), and often unusually fast, heartbeat. It means that the heart may not be pumping as well as it should. As a result, blood clots are more likely to form in the heart, increasing the risk of having a stroke (blood supply to part of the brain is cut off caused by a blockage [from a blood clot] in one of the blood vessels or by a bleed in the brain).
AF makes your risk of a stroke five times higher so it is important that you get the right treatment to control your heartbeat, and reduce your risk of stroke.
How does AF affect the heart?
The heart is a muscle that pumps blood around your body.
- It is made up of four chambers: the two upper chambers are called the left and right atria, and the two lower chambers are called the left and right ventricles.
- The atria send electrical signals that cause the heart to beat. The ventricles pump blood to the lungs and around the body.
- AF is an abnormal heart rhythm that occurs when the heart has problems signalling correctly. As a result, the heart cannot pump blood as regularly or as efficiently as usual.
- As the blood is not being pumped efficiently, this can sometimes cause blood to pool in the upper chambers (atria) and form a blood clot.
- If this occurs and a clot (or bits of a clot) break loose, they can travel through the bloodstream. If a blood clot blocks blood flow to the brain, it may cause a stroke.
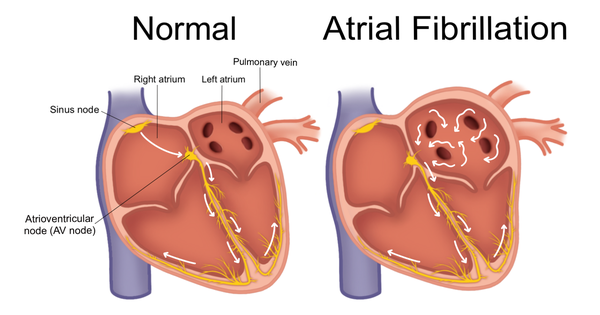
White arrows represent the electrical activation through the yellow conduction system resulting in a heartbeat/contraction. (Image credit: Olivia Rumsey, with permission by ClubAfib)
How does it feel to have AF?
Sometimes AF does not cause any symptoms, and a person with AF may be unaware that their heart rate is irregular. Those who do have symptoms may sometimes feel:
- Palpitations (racing heart)
- Tired or exhausted
- Shortness of breath
- Chest pain
- Weakness
- Faint, dizzy or lightheaded
- Less able to exercise
What factors increase the risk of stroke?
Anyone (at any age) can have a stroke. The risk of stroke will increase for:
- Older age
- Certain medical conditions such as AF, high blood pressure, diabetes, high cholesterol
- Family history of someone who has had a stroke
- Overweight / unhealthy diet
- Smoking
- Too much alcohol (above recommended limits)
How is AF treated?
You may require treatment to help your heart beat more effectively, change your heart rhythm back to normal and reduce your risk of stroke. Your doctor will talk to you about which treatment will be best for you.
Reducing the risk of AF-related stroke
Anticoagulant medication, known as a ‘blood thinner’, is used to reduce the risk of stroke due to AF by slowing down the clotting process and making a blood clot less likely to form.
You will be risk assessed to see if anticoagulant medication is appropriate for you, along with their risks and benefits.
Anticoagulant medication
Your doctor will select the appropriate anticoagulant medicine for you. The choice of anticoagulant medication will be based on various factors e.g. kidney function, body weight, other medications that you are taking, bleeding risk. Always keep the patient alert card with you (eg wallet).
My anticoagulant medication
Indication: Atrial Fibrillation (AF)
Anticoagulant agent and dose: _______________________________
What should you know about your anticoagulant medication?
Take the anticoagulant medicine exactly as prescribed by your doctor/pharmacist and do not miss any dose(s).
Do not stop taking your medication without discussing it with your doctor/pharmacist as the risk of blood clots may increase.
Tell your healthcare provider about any other medicines you are currently taking, took recently, or intend to start taking before you start this medication.
Tell your healthcare provider that you are taking an anticoagulant medication before any surgery or invasive procedure (including dental procedure).
What are the main possible side-effects?
Like any medicine, anticoagulants may cause side effects. Anticoagulant medication can increase the risk of bleeding and bruising. Side-effects may include:
- More bleeding than usual from the nose or gums
- Blood present in urine (bright pink, red or dark brown blood)
- Blood present in stools (bright red, dark brown or tarry black stool)
- Blood present in vomit (bright red or dark brown vomit, or looking like coffee grounds)
- Bleeding when coughing
- Heavier menstrual periods than usual
Note: Seek immediate medical advice from your GP or go to your nearest Emergency Department if you experience a head injury or any severe or recurrent bleeding-related side-effects, especially in your urine, vomit or stool.
Who can you contact if you have any concerns or need further information
Your General Practitioner (GP) will be informed that you have atrial fibrillation, and the treatment started by the hospital.
If you are worried about any new or worsening symptoms then you should seek medical advice urgently from your GP, NHS 111 (24/7) or your nearest Emergency Department.
Further information can be found from the NHS website, British Heart Foundation website, Stroke Association website, and Atrial Fibrillation Association website.

