Oesophageal Stent Insertion
This leaflet has been written by staff working in the Endoscopy Unit at Chelsea and Westminster Hospital.
We hope you find it useful. If, after you have read it, you have any questions or concerns, please ring us on our direct line 020 3315 3056/5223.
When you come into the Unit (2nd Floor, Lift Bank B), please talk to us about any worries and ask any questions you have.
If you would like to change your appointment time or date, please contact the Endoscopy Unit booking team on 0203 315 4141/5984 or email us: caw-tr.diagnosticteamadmin@nhs.net
Your appointment time in Endoscopy is approximate because some procedures may take longer than expected and emergency procedures need to take priority. Please expect to be in the department for several hours – having pre-procedure checks, the procedure and for recovery after the procedure.
What is an Oesophageal Stent?
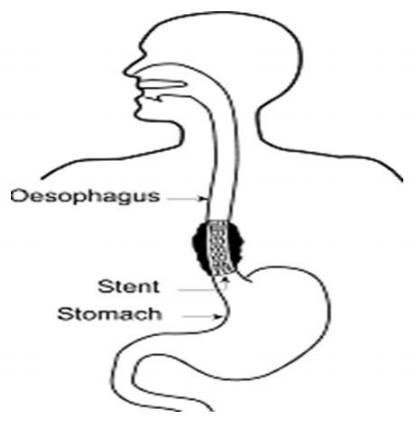
The Oesophagus (gullet) is a hollow muscular tube which takes food from the throat down to the stomach. This can become blocked/narrowed due to cancer or scarring – this would then lead to difficulty swallowing.
An Oesophageal Stent is an expandable mesh metal tube which can traverse the narrowing/blockage in the oesophagus/gullet, such that food and drink can then pass through into the stomach.
The procedure is performed with you sedated. An endoscopy is performed to assess the blockage, then using X-ray as a guide, a wire is advanced through the blockage into the stomach. Over this wire the stent (at this point constrained by a narrow plastic sheath) is advanced within the narrowing, and the stent is deployed using X-ray guidance.
What should I expect after the procedure?
You may experience some chest discomfort / pain after the procedure as the stent gradually expands, however this usually settles over a few days.
Depending on where exactly the narrowing in your oesophagus/gullet is and where the stent is placed you may experience reflux/heartburn after the procedure long term. After the procedure the medical team may therefore prescribe medication to limit this, and recommend avoiding lying flat / sleeping with the head of the bed elevated.
The team will advise you on diet following stent insertion, but in general you will be allowed fluids after a few hours, gradually building up to a soft/moist diet over days.
What should I do before I come in?
You should not eat or drink anything for 6 hours before the procedure, sometimes the medical team may advise a longer time without solids before.
As you will be having sedation, you must organize for someone to take you home after the test and be with you for 24 hours.
Please remove any nail polish prior to attending as this can interfere with readings on our oxygen monitoring devices.
Drugs
If you are diabetic please let us know in advance.
Unless advised otherwise, if you are taking any of the following medicines, please inform the pre-assessment nurse or a member of the Endoscopy team for further instructions:
- Warfarin, rivaroxaban, apixaban, dabigatran, edoxaban
- Clopidogrel, prasugrel, ticagrelor, dipyridamole
- Any other medication used to thin the blood
Are there any risks or complications?
Oesophageal stent insertion is a very safe procedure but as with any medical treatment there are some potential risks and complications that can arise:
Pain: approximately 10% can have chest pain after the procedure as the stent opens up, usually this eases after a few days
Reflux/heartburn: Can occur especially if stent crosses into the stomach: medication/advice may be given to treat this
Stent migration/blockage: Sometimes stents can migrate/ slip at a later date, or become blocked with tissue growth, in this case further procedure(s) may be required at a later date.
Infection: Small risk of chest infection after the procedure
Bleeding: It is possible that a little bleeding may occur during the procedure but this usually stops without the need for any action, rarely significant bleeding may occur requiring blood transfusion
Perforation: The risk of perforation / tear is very small (<1%). Some patients can develop perforation or fistulation into surrounding organs such as the lungs or breathing tubes, some time after stent insertion, in the setting of cancer.
Dental: Very small risk of damage to teeth/dental work.
Sedation for the procedure
Sedation (given through an intravenous cannula) will be required for you to tolerate the procedure, and enable an adequate quality of treatment to be completed.
The type of sedation required for your procedure will depend upon several factors including the anticipated complexity of the procedure and your other medical problems. The medical team will determine this prior to your booking. If they determine that a general anaesthetic is necessary, you may need to be assessed by an anesthetic doctor prior to the procedure.
Please note that after receiving sedation or General anaesthesia, even if you feel wide awake your reactions may still be affected. You may find it difficult to concentrate and you may forget things that you have been told after the procedure. The nurses will give you written discharge information. This includes the advice that for 24 hours after sedation you should not drive, ride a bicycle, operate machinery, take sedatives or drink alcohol, or sign legal documents.
After the procedure an escort must collect you from the unit, take you home and be with you for the next 24 hours. We cannot escort you home.
What will happen when I come in?
On admission to the unit a nurse will ask you several questions about your health, current medication (please bring an up to date list with you), take your blood pressure and pulse, and ask you to get changed into a gown.
Please leave any valuables at home, as we cannot be responsible for any valuables lost whilst you are in the unit. You do not need to bring anyone with you to your appointment, unless they are acting on your behalf (e.g. interpreting for you). Your escort/relative will only be needed when you are discharged if you have sedation.
Prior to the test you will be seen by the endoscopist. This is an opportunity to discuss the test before you sign a consent form. Please ask any questions you may have. It is important that you understand what is going to happen.
Please note that you may have to wait for some time on the day of your procedure as occasionally there are emergency inpatient cases which need to be accommodated. Rarely there may be a need to rearrange your procedure for another date, we will do anything possible to avoid this if at all possible.
FAQs
Q: Will I get the results of my test on the same day?
A: Before you go home you will be given the results of the test. It will also say whether you need an appointment with a consultant or with your GP. Your GP will receive a copy of the report of the examination from the hospital. If biopsies were taken these results take longer and will be sent to your consultant and GP.
What happens to my medication?
We will talk to you before you go home about any changes/additions to your medications.
You may be prescribed painkillers and medication to limit reflux.
What can I expect when I go home?
You may feel bloated if some air remains in your stomach. It is advisable to sit upright and if possible walk around to help relieve this. Warm drinks and peppermints will also help you to pass the wind. You may have a sore throat, which can last up to 48 hours. Taking throat lozenges will help. Pain relieving tablets such as paracetamol may be taken according to manufacturer’s instructions.
You may have chest discomfort/pain, and/or symptoms related to reflux after insertion of the stent.
If you have worsening severe pain not settling with pain killers or evidence of bleeding (vomiting blood / passing altered blood or jet black motions when you open your bowels) please contact the Endoscopy Unit from 8am–6pm on 020 3315 3056/5223 or go to your nearest Accident and Emergency and remember to take your Endoscopy report with you.

