Intermittent Pneumatic Compression to Reduce the Risk of Venous Thromboembolism
Intermittent Pneumatic Compression (IPC) This leaflet has been produced by the hospital Thrombosis and Thromboprophylaxis Group to explain how IPC in hospital can help to prevent blood clots. It will also discuss the signs and symptoms of blood clots. We hope it answers some of the questions you may have.
Venous Thromboembolism (VTE)
VTE is where a blood clot (called a thrombus) forms in a vein which can block off or reduce blood flow. The most common form is a blood clot in the deep veins of the legs known as a deep vein thrombosis (DVT). The DVT can break off and travel to the arteries of the lung where it will cause a pulmonary embolism (PE). DVT and PE are known under the collective term of VTE.
Mechanical Thromboprophylaxis
Patients who have reduced movement whilst in hospital, for example after surgery, recent stroke, are at an increased risk of developing blood clots.
What is Intermittent Pneumatic Compression (IPC)?
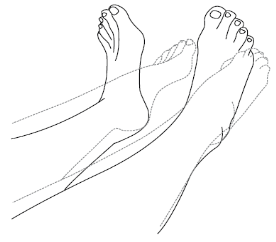
IPC is a common mechanical device applied to the lower legs to help reduce the risk of you developing a blood clot whilst in hospital.
IPC increases the blood flow in your legs and helps to reduce the risk of blood clots developing whilst you have reduced mobility
How does IPC work?
The IPC sleeves are applied to the legs, and gently inflate and deflate to apply compression to the legs – often in the sequence starting with the ankle, then the calf and finishing with the thigh.


How long do you need to wear IPC for?
Your doctor or nurse will advise when you can stop wearing the IPC sleeves, but they are usually worn for 24 hours a day.
You do not need to continue to wear the IPC sleeves after you leave hospital.
The sleeves will be removed daily for showering, to allow staff to assess your skin condition and for any physiotherapy.
Please ask your nurse to explain anything you do not understand
What should you do if you experience problems when wearing the IPC sleeves?
Please inform a staff member if:
- The sleeves are not inflating regularly or if you suspect the machine has been switched off
- The sleeve feels either too tight or too loose
- If you start to feel numbness, pins and needles or increased pain in your foot
What can you do to help reduce your risk of blood clots?
You can help reduce your risk of developing a blood clot by:
- Drinking plenty of water to keep hydrated
- Carry out some leg exercises whilst lying in bed
- Lying on your back or sitting
- Bend and straighten your ankles quickly 10 times
- Keep your knees straight during the exercise to stretch your calf muscles
How will you know if you have DVT or PE?
The symptoms of DVT in the leg include:
- Swelling
- Pain
- Warm skin
- Tenderness
- Redness (particularly at the back of your leg below the knee)
In some cases, there may be no signs or symptoms of DVT at all in the leg
The symptoms of PE include:
- Shortness of breath
- Pain in your chest that is worse when you breathe in
- Collapse (in severe cases)
Both DVT and PE are serious conditions that require urgent investigation and treatment. If you suspect you may have DVT or PE, you should seek medical advice immediately either from your GP or nearest A&E (Emergency Department)
Who can you contact for more information?
If you would like any more information or have any questions, please ask a doctor, nurse or pharmacist. Further information can be found from NHS website www.nhs.uk or Thrombosis UK www.thrombosisuk.org.

