Dietary advice for Gestational Diabetes
Introduction
A healthy diet is an important part of a healthy lifestyle at any time but especially for women who are pregnant or planning a pregnancy. Sometimes pregnant women develop a type of diabetes where their blood glucose level starts to rise which can cause their baby to grow larger than the gestational size which can cause complications if not managed. Your midwife & obstetrician will normally discuss this further with you.
What is Gestational Diabetes (GDM)?
Gestational Diabetes (GDM) is the name given to diabetes that can occur during pregnancy (Gestation). Diabetes is an inability of the body to control the amount of sugar (glucose) in the blood.
Some known risk factors for developing gestational diabetes.
- A body mass index of above 30 kg/m2
- Maternal age of 30 years or over
- A history of polycystic ovary syndrome (PCOS)
- A previous baby weighing 9.9lbs (4.5kg) or more.
- A family history of type 2 Diabetes
- Some ethnic groups (African, African-Caribbean and Asian) are more susceptible.
- Weight gain between pregnancies
Blood Glucose Targets for GDM
- Before breakfast: Below 5.3 mmol/L
- One hour after each main meal: Below 7.8 mm ol/L
How can I control my blood glucose with GDM?
- Diet & lifestyle changes is the first line management for GDM
- Follow a healthy balanced diet, in particular balancing the macronutrients like carbohydrates, protein & fats can make a difference to your blood glucose post meals.
- Making simple changes to the food choices & portion sizes can help with controlling blood glucose.
- Sometimes eating patterns & food choices may need to be adjusted to improve blood glucose.
- Physical activity especially after eating can help lower blood glucose levels.
Which food and drink cause my blood glucose levels to rise?
What you eat and drink has a key role in managing your blood glucose levels during pregnancy. The right balance of a variety of food is also important to make sure you and your developing baby get the nutrition you both need.
There are three main nutrients in the food/drink that we consume: Carbohydrate, Protein and Fat.
Carbohydrates have the biggest impact on our blood glucose levels. They are the body’s preferred source of energy and can provide fibre as well as other vitamins so try not cut them out completely. There are two main types: Sugars and starches.
Sugars
- All fruit—fresh and dried
- Fruit juices
- Natural syrups—maple, honey, agave, jaggery, molasses
- Milk
- Yogurt
- Ice cream
- Custard
- Table sugar—white, golden and brown
- Confectionary
- Fizzy drinks
- Cakes
- Biscuits
- Chocolate
- Sweets
- Desserts
Starches
- Bread
- Pasta
- Noodles
- Rice
- Flour
- Chapatti
- Couscous
- Polenta
- Quinoa
- Oats
- Oat cakes
- Rice cakes
- Cereals
- Potato
- Sweet potato
- Parsnips
- Swede
- Beans
- Lentils
- Peas
- Sweetcorn
- Yam
- Idli
- Dosa
- Green bananas
- Plantain
- Cassava
- Fufu
- Manioc
The effect on blood glucose levels depends on the amount and type of carbohydrates eaten.
Glycaemic Index (GI)
All food that contains carbohydrate have a glycaemic Index value (GI). This describes the speed that the body breaks down carbohydrate into glucose and absorbs it into the blood. Low GI foods are the best choices as they are absorbed and raise the blood glucose more slowly so can help to keep your blood glucose levels within the healthy range & regulate your appetite much better. High G.I. foods are absorbed quicker and raise the blood glucose quickly. Therefore, can be problematic if you have GDM.
Table below shows you some examples of Low GI and High GI foods.
Low GI
- Plain rolled Oats.
- No added sugar Muesli
- Oat flakes no added sugar.
- Wholegrain breads: Granary, multigrain, other seeded varieties
- Rye bread, pitta bread, sourdough bread and chapattis
- Basmati & brown rice
- Wholegrain pasta & noodles
- New potatoes
- Sweet potatoes
- Beans, lentils, such chickpeas, kidney beans, and butter beans
- Plantain, yam, green banana
- Couscous, Bulgur wheat and Quinoa
High GI
- All refined cereals, such as cornflakes, rice crispies, crunchy nut cornflakes, coco pops
- White bread
- Muffins
- Biscuits
- Cakes
- Sugar
- Honey
- White rice – easy cook variety
- Fries
- Normal fizzy drinks
- Fruit juices
Portion size for carbohydrates (carbs)
When eating carbs, remember these four key principles:
- Watch your portion sizes (the amount on your plate)
- Choose higher fibre low GI options, as they generally tend to release the glucose slowly and keep you fully for longer, they also help with constipation.
- Avoid food and drinks containing added sugar.
- Pair your carbs with protein and healthy fat, this will help lower the GI of the carbohydrate food further.
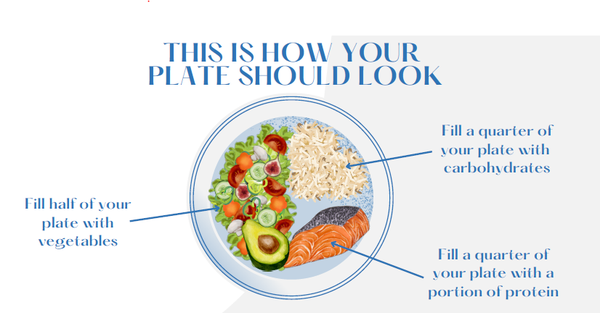
Aim to have no more than one fist sized portion of cooked starchy carbohydrate in each meal, for e.g. 2-3 egg sized potatoes OR 3-4 tablespoons or a small cup of cooked pasta/noodles/rice OR 2 slices of bread OR 1-2 small high fibre chapattis. This portion size will roughly be around 30 – 50g carbs in a main meal.
Generally counting the amount of carbs in your meals is not necessary, however if you find it helps, as a guide, per meal:
Breakfast: 30- 40g total carbs (if you become more insulin resistant in the morning, you may need to either split your breakfast or lower the total carbs)
Lunch: 40 – 50g total carbs
Dinner: 40 – 50g total carbs
Snacks: 10 – 15g
Note: This is just a guide, everyone has different degree of insulin resistance with their GDM. By regular blood glucose monitoring you’ll be able to adjust your diet accordingly.
Resources that can help with carb counting
- Food labels, look at Nutritional info at the back of packets and look at total carbs per portion you are eating.
- Internet search, look for carbohydrate information in the portion of food you are eating.
- Carbs & Cals book or App can help by giving you a visual guide to raise awareness during your pregnancy & post-delivery.
Fruit & Vegetables
- These provide variety to your diet.
- Good source of vitamin C, micronutrients and minerals
- Fibre – bowel health (helps prevent constipation)
- Avoid excessive amount of fruit, although generally a healthier choice snack, too many can raise blood glucose.
- Try instead, a fist size portion for e.g., 1 handful of berries or 1 slice of a larger fruit, you can combine this with some protein food such as cheese or handful of nuts (see protein section below) which will provide you with protein & some good fat as well as stopping a rise in glucose.
- One portion of fruit can be a healthy snack in between meals, when you feel hungry, for e.g. Generally aim for 2 portions of fruit per day
- 1small – medium apple/orange/pear
- x2 small fruit; plum or satsuma
- small handful of berries
- Veg/salad be more generous, as they have very little impact on your blood glucose levels, aim for half your plate, as it helps with keeping you fuller for longer, they provide variety and bulk to a meal.
- Frozen & Fresh vegetables are equally beneficial.
Protein
Protein foods include meats, eggs, chicken, fish, seafood, cheese, yoghurt, milk, non-meat origin: Tofu, Soya, Quorn, beans, lentils, nuts.
- These are important for growth, tissue repair, and maintenance & hormone production.
- They help lower GI of your meals and help keep glucose levels in range.
- Improve satiety.
- Aim to include 1 portion at every mealtime, choose leaner cuts, for e.g., 1 skinless chicken breast/ piece of fish, a small cup of cooked lentils, a handful of nuts.
- Ensure all your meats/chicken/fish are well cooked to avoid contamination.
- Aim for x2 portions of oily fish/week, a portion is: a piece of fresh salmon or 1 tin of mackerel or sardine.
Fats
Some dietary fats are important, as we need them for energy, to make hormones and for our cell membranes. However, too much can contribute towards the total amount of calories we consume. You don’t need to avoid them; you need to exercise moderation and choose the good fats over the processed varieties.
There are 3 main types of dietary fats:
Saturated
- Mostly from fatty & processed meats like sausages & salamis, pies, pastries anything cooked in lard
- Clotted Cream
Monounsaturated
- Also known as Omega 3 fats
- High level in avocado, olive, rapeseed, ground nut oil, seeds & nuts
- Also, high quantity in a Mediterranean diet
Polyunsaturated
- Also known as Omega 6 fats
- Seeds & nuts, oils
- Oily fish like salmon, sardines, mackerel, trout (in pregnancy the current recommendation is x2 portions of oily fish per week)
Key messages
Fat is important in our diet but watch the amount as they are also high in calories which can lead to excess weight gain during pregnancy.
- Watch the amount you add to food.
- Limit intake of saturated fat partial substitution with good fats such as monounsaturated and polyunsaturated
- Fats can help lower GI of meals, for example putting peanut butter or avocado on toast for breakfast.
Meal pattern
Try to eat regular meals (breakfast, lunch and evening meal). Spreading your intake over the day can help to manage your blood glucose levels. If you skip meals, you might be more likely to overeat at the next meal or end up on snacking on things that can have a big impact on your blood glucose.
Avoid eating carbohydrate late in the evening. Having your dinner too late at night can affect your fasting blood glucose the next day. If you can, try to have your dinner before 8pm. If you need to snack after dinner, opt for low carb options e.g., nuts, cheese, small portion of Greek yogurt.
| Meal 1 | Meal 2 |
|
Breakfast Options:
|
Breakfast Options:
|
|
Mid-morning snack ideas:
|
Mid-morning snack ideas:
|
|
Lunch:
|
Lunch:
|
|
Mid-afternoon:
|
Mid-afternoon:
|
|
Dinner:
|
Dinner:
|
| Bedtime: A sugar free drink or plain glass of milk, stick with protein food if hungry | Bedtime: A sugar free drink or plain glass of milk, stick with protein food only |
Examples of snacks containing around 10 – 15g carbs/ portion
| Food | Amount | Food | Amount | Food | Amount | ||
| Corn on the cob | 1 – 2 small pieces | Hummus + Rye/Pumpernickel bread | 1 slice | Diet or plain natural yoghurt | Small pot | ||
| Plain wholegrain crackers | 1 - 2 | Plain popcorn (no sugar) | 30 g /small handful | Small Samosa | 1 | ||
| Piece of fruit, e.g. apple/banana |
1 small- medium |
Fresh berries | 1 handful | Plain milk | 1 glass |
Examples of snacks with very low carbohydrate content
| Food | Amount | Food | Amount | Food | Amount | ||
|
Nuts/Seeds |
small handful | Char-grilled vegetables | One large handful | Raw vegetables with low fat savoury dip | Large handful | ||
|
Meat, chicken, fish (use caution with coating) |
e.g., A slice ham / cooked chicken |
Cream cheese (e.g., Cottage cheese) | 30 – 40 g | Avocado |
1 small |
||
| Boiled egg | 1 | Firm cheese e.g. cheddar | 1 match box size or slice |
Cheese strings or baby bel |
1 serving | ||
| Sugar free jelly | 1 pot |
Olives |
Small handful | Unsweetened almond milk/soya milk | 200 mls |
Food safety in pregnancy
There are certain foods that are best to avoid while you are pregnant as they can put your baby’s health at risk. These include some types of cheese and raw or uncooked meat. For more details, please see websites below.
- Health Eating in Pregnancy—Start4life
- Food Safety in Pregnant Women—FDA
- Foods to Avoid in Pregnancy—NHS
Exercise in pregnancy
- Exercising during pregnancy has been shown to have many benefits, including reducing stress and anxiety, improving sleep patterns. Please check with you doctor if you are experiencing any discomfort or bleeding.
- Exercise can also help your insulin work more effectively, which keeps your blood glucose level under control, especially walking or being more active post eating.
- For more information on this please check:
‘Exercise in Pregnancy’ Royal College of Obstetricians and Gynaecologist, 2006. NICE ‘Diabetes in Pregnancy’ July 2008.
In summary
- Eat three regular meals every day.
- If hungry in between meals aim for a small snack containing carbohydrate between 10 – 15g (preferably low GI) or have a carb free snack,
- Avoid large meals – spread your carbohydrate portion as evenly as possible over the day.
- Try not to miss meals as you are likely to eat more later.
- If appetite is poor aim for little and often for e.g. a yoghurt with fruit &nuts
- Balance your main meals with other nutrients coming from lean meat, fish, chicken or meat alternatives and plenty of salads/vegetables.
- Ensure your meat, fish, chicken or other sea foods are well cooked.
- Ensure good fluid intake, aim for 2 litres of sugar free fluid per day, water and tea without sugar also counts towards your daily fluid intake. This will help avoid or relieve constipation.
- Choose lower carbohydrate toast toppings such as peanut butter, cheese, marmite, and avocado instead of jam, marmalade, and honey.
- Avoid highly processed breakfast cereals such as cornflakes or crunchy nuts as these can cause blood glucose to rise rapidly.
- Protein foods do not cause your blood glucose to rise, so opt for a larger serving of lean meat, fish, eggs, nuts at meals if you are hungry.
- Exercise is important in pregnancy so aim for 30 mins of exercise daily. For instance, 15 – 20 minutes’ walk or longer after meals will help to control your blood glucose.
Post delivery care
Most women return to normal blood glucose levels as soon as their baby is born. Usually, 6 weeks after delivery you will be asked to take an appropriate blood glucose test to confirm that you no longer have diabetes.
You should continue making healthier food choices and exercise regularly to help you achieve and maintain a healthy weight. This is important as you are at more risk of developing diabetes later in life if you have had it during pregnancy.

